Abstract
Background: Chronic constipation leading to fecal impaction and stercoral perforation is an important cause of morbidity and mortality in the aging population. Gangrenous cystitis, an even more rare entity, previously reported primarily in obstetric cases, has not been reported in association with stercoral perforation until this report.
Summary: This case report details the clinical presentation and treatment of a 61-year-old female with history of end-stage renal disease and history of kidney transplantation who presented in septic shock with a positive urinalysis. She underwent an emergent computed topography scan of the abdomen and pelvis which demonstrated a perforation originating from the sigmoid colon. Damage control surgery was performed, the sigmoid colon was resected, and the intestine was left in discontinuity. The abdomen was left open with a temporary abdominal dressing and a catheter for direct peritoneal resuscitation. She returned for a “second look” laparotomy where ischemic bladder tissue was noted. A partial cystectomy was performed, and the bladder was reconstructed over a Foley catheter and her abdomen remained open for continued direct peritoneal resuscitation. Ultimately, the
family determined that this level of care was not consistent with the patient’s wishes and she was made comfort measures.
Conclusion: This is the first report of stercoral perforation of the sigmoid colon in association with gangrenous cystitis in the literature. This case report highlights the importance of a thorough evaluation of the pelvis during surgical management of stercoral perforation so as not to miss concurrent gangrenous cystitis.
Keywords
sepsis, sterocoral perforation, gangrenous cystitis
Introduction
Gangrenous cystitis is a rare condition that has only been reported in the literature a total of 240 times worldwide since 1934. It was once seen in obstetric cases, associated with labor and delivery, but is now most commonly secondary to pelvic radiation/surgery, chemotherapeutic agents, urinary retention, urosepsis, pelvic thrombophlebitis, and colovesical fistulae. The pathogenesis is unknown but is thought to be initiated by bladder ischemia that is then subject to microbial superinfection [1] . Fecal impaction secondary to chronic constipation can lead to Stercoral Perforation (SP) through pressure necrosis of the large bowel [2]. SP is a well-defined entity in the literature that is associated with significant morbidity and mortality and has also been associated with a prior history of renal transplantation [3]. This case report is the first to identify SP of sigmoid colon as a cause of gangrenous cystitis.
Case History/Examination
The patient is a 61-year-old female with a history of End Stage Renal Disease (ESRD) and remote kidney transplantation, with recent admission to the hospital for intertrochanteric fracture after fall. She was subsequently discharged to a rehab facility after a surgical repair of the fracture. The patient presented to our hospital two weeks later in septic shock. On physical examination she had an altered mental status, she was in respiratory distress, and profoundly hypotensive. The abdominal examination was remarkable for a soft but distended abdomen and a palpable transplant kidney in the right lower quadrant with no peritoneal signs.
Investigations and Treatment
White blood cell count was 11,000 with 94% neutrophils and serum lactate was found to be 6.1 cells per cubic millimeter of blood. A Urinalysis (UA) was grossly positive Urinary Tract Infection (UTI) so the patient was transferred to the Medical Intensive Care Unit (ICU) for suspected urosepsis. The patient was intubated and fluid resuscitation along with empiric broad spectrum antibiotics were initiated. An emergent Computed Tomography (CT) scan of the abdomen and pelvis was obtained and showed radiological evidence of perforated viscous, most likely from the sigmoid colon (Figure 1).
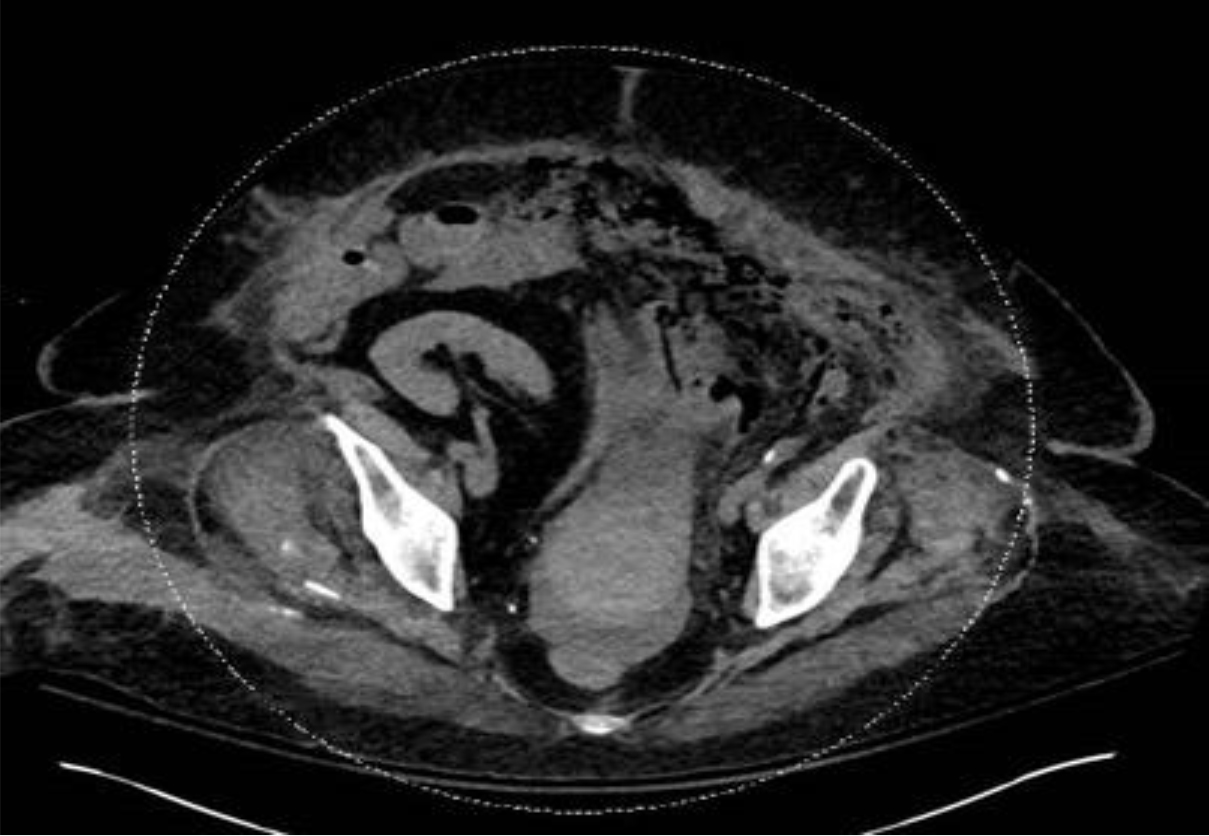
Figure 1. CT scan of the abdomen and pelvis showing significant stranding and multiple locules of air outside the bowel lumen in the left lower quadrant adjacent to the sigmoid colon and along the left paracolic gutter.
An emergent surgical consult was obtained and the patient was taken immediately to the operating room for exploratory laparotomy. Upon entry to the abdomen, there was foul smelling, turbid fluid and an ischemic, dilated proximal sigmoid colon was encountered. A stercoral perforation of the sigmoid colon on the mesenteric border into the retroperitoneum was noted. The left side of the retroperitoneum had a large amount of necrotic tissue extending into the pelvis.
A damage control surgery was performed. The sigmoid colon was resected, and the intestine was left in discontinuity. The left side of the retroperitoneum and pelvis were opened, and debridement of the necrotic retroperitoneal tissue was performed. A 19 Fr blake drain was placed intra peritoneally for direct peritoneal resuscitation [4, 5]. At the end of the case, the patient was transferred to the Surgical ICU for further resuscitation and correction of metabolic abnormalities.
Postoperatively, the patient’s hemodynamics improved transiently, and vasopressor requirement did decrease somewhat but her serum lactate level continued to rise. With a new elevation of serum lactate the patient was taken to the operating room for a “second look” laparotomy approximately 24 hours later. No further bowel ischemia or necrosis was noted. There was still a significant amount of retroperitoneal necrotic tissue, especially in the pelvis. Further dissection into the pelvis did reveal a 7 cm cystostomy with ischemic bladder tissue mostly on the left side with clear demarcation of ischemic changes. There was some ischemia of the right side of the bladder as well. A Urology and Transplant Surgery consultation were obtained due her history of kidney transplant.
Outcome and Follow-Up
A multidisciplinary discussion resulted in the decision to perform a partial cystectomy and not explant the donor kidney. All of the obvious necrotic tissue was then resected, and the bladder was reconstructed over a Foley catheter. Afterwards, since the patient still was in a profound state of shock, the patient’s bowel was left in discontinuity, the abdomen was temporarily closed, and the patient was transferred back to the Surgical ICU for further management.
The next day the patient underwent a planned relaparotomy with abdominal wash out and temporary abdominal closure. No further areas of bowel or bladder necrosis were noted. Due to the patient’s extensive comorbidities and lack of improvement over the following 48 hours as well as the extent of the care she would continue to require, the family felt this was not consistent with her wishes and elected to make her comfort measures. The patient passed away shortly thereafter.
Discussion
This is the first case report of bladder necrosis due to stercoral perforation of the sigmoid colon. With no literature to guide us, it is difficult to make absolute conclusions, but we believe that the stercoral perforation into the retroperitoneum led to an inflammatory reaction and local infection around the bladder leading to ischemia and gangrenous cystitis.
In the literature, there are numerous causes of bladder necrosis published, mostly in the pre-antibiotic era. These causes include prolonged labor, pelvic radiation, chemotherapy, urinary retention, urosepsis, and pelvic thrombophlebitis to name a few. In these published cases, the mainstay of treatment has been early antibiotic therapy and surgical treatment with extensive debridement of necrotic bladder and wide drainage [6, 7].
In this case report, we differed from the traditional management in that we performed a damage control laparotomy with temporary abdominal closure and direct peritoneal resuscitation. This strategy allowed for source control in the OR and rapid transfer to the ICU for further resuscitation and correction of metabolic abnormalities. This provided our patient with the best chance of survival. Ultimately, it was her wishes that she would not want to live if she were not guaranteed to return to her former quality of life, and she was made comfort measures. However, we believe that she most likely would have survived this hospitalization had this been in line with her wishes.
Conclusion
Whether this patient’s bladder necrosis was due to her stercoral ulcer or her septic shock remains unclear as the literature is equally vague regarding both topics. However, surgeons should be aware of this phenomenon and while operating on the bowel emergently for perforation, should take the time to assess the pelvis, especially in patients with a grossly positive urinalysis.
Lessons Learned
Stercoral perforation of the sigmoid colon leading to septic shock can be associated with gangrenous cystitis and necessitates a thorough evaluation of the pelvis while operating on this entity.
References
- De Rosa A, Amer T, Waraich B, Bello A, Parkinson R (2011) Gangrenous cystitis in a 42-year-old male. BMJ Case Reports 2011: 1–4. [Crossref]
- Chakravartty S, Chang A, Nunoo-Mensah V (2013) A systematic review of stercoral perforation. Colorectal Disease 15: 930–935. [Crossref]
- Dubinsky I (1996) Stercoral Perforation of the Colon: Case Report and Review of the Literature. Journal of Emergency Medicine 14: 323–325. [Crossref]
- Rai R, Sikka P, Aggarwal N, Shankaregowda SA (2015) Gangrenous Cystitis in a Woman Following Vaginal Delievery: An Uncommon Occurrence -A Case Report. Journal of Clinical and Diagnostic Reasearch 9: 13–14.
- Smith JW, Neal Garrison R, Matheson PJ, Harbrecht BG, Benns MV, et al. (2014) Adjunctive treatment of abdominal catastrophes and sepsis with direct peritoneal resuscitation: indications for use in acute care surgery. J Trauma Acute Care Surg 77: 393–398 [Crossref]
- Hinev A, Anakievski D, Krasnaliev I (2010) Gangrenous Cystitis: Report of a Case and Review of the Literature. Urologia Internationalis 85: 479–481. [Crossref]
- Piraprez M, Ben Chehida M, Fillet M (2017) Case Report: Emphysematous cystitis. Red Med Liege 384–387.