Introduction
The use of intra-radicular restraint systems for complete dentures, has been indicated as a viable option for decades ago, and have been called “overdentures” [1–6]. The overdentures concept is not new in dentistry and has been used since the 70’s years. Actually, considering its potential benefits, there has been a reduction in the indication over natural supports [2,4,5].
Flaws in the control of dental caries and periodontal disease, possibility of root fractures and the difficulty in understand and reproduce the bilaterally balanced occlusion, takes many professionals to be reluctant to indicates this technique, preferring to remove remaining teeth and install implants [3,4,6]. However, the use of natural tooth roots to support overdentures brings benefits to the patient, assisting the proprioception, eliminating the osseointegration period and reducing the final cost of the prosthesis, because it eliminates the need for the acquisition of prosthetic components, and clinical and laboratory procedures related to installation of implants. Maintaining compliance with oral hygiene and specific care with the natural supports and prosthesis, the time life justifies the indication of this technique. In addition, an appropriate treatment plan for the making of overdentures on natural roots is a mandatory choice for patients who have underwent radiotherapy as a complementary treatment of cancerous lesions. Several authors are unanimous in stating that the radiation is a factor associated with the loss of implants and the decrease in its survival rate [7–16]. The effects of the radiotherapy appear to be more severe in the jaw due the less blood supply in the newly formed bone. So the benefit of the indication of the overdenture on natural roots in these cases, when compared to the overdenture on implant must overcome risk [7].
Patients with changes in the occlusal plane due to absence or inadequate dental position tend naturally to have changes in mandibular positioning, in both vertical (vertical dimension of occlusion) and horizontal plane (distal displacement, midline deviations). Clinical researches have been indicated the use of occlusal devices, occlusal appliance, as a valid resource for the normalization of mandibular position. These devices can be adapted in the superior dental arch on the remaining teeth or alveolar ridge and must be flat and smooth occlusal surface [17–19]. These occlusal devices act as facilitators of the mandibular repositioning, by blocking all or part of the proprioceptive stimuli responsible for the control of masticatory activity, in establishing an ideal position for prosthetic rehabilitation [19,20].
Clinical Case
A male patient, 58 years old, in need of prosthetic rehabilitation, attended the Centre for the Study and Treatment of the Functional Changes of the Stomatognathic System – CETASE, of the School of the Dentistry of Piracicaba – UNICAMP/Brazil, in August 2015, three years after had been submitted to surgical treatment for the removal of a moderately differentiated ulcerating spin cell carcinoma (grade II) in the larynx. The medical history revealed that, in 2004, after the differential diagnosis had been performed, was submitted to supraglottic laryngectomy and cervical bilateral radical deflation followed by postoperative radiotherapy. The treatment was finished in November of the same year. The following year the patient underwent gastrectomy due to a primary tumor of stomach. Three years after they were found metastases in the regions of the base of the tongue and mandible jaw, being subjected to glossopelvemandibulectomy, removing part of the base of the tongue, right inferior part of the mandibular ramus (Figure 1) and the superficial and deep masseter muscles, tendon of the temporal, lateral and medial pterygoid muscles and ligament stylomandibular of the same side. He was not subjected to facial reconstruction and to supplementary feed, used an intestinal bowel probe.

Figure 1. Panoramic radiograph showing the complete absence of the mandible branch of the right side due to the removal of the cancerous lesion.
Dental history began to be recorded in 2016, through the use of the Clinical Chart of CETASE, with the goal of identify signs and symptoms of TMJ disorders, according of the severe mandibular misalignment in horizontal and vertical plane. Facial asymmetry with severe jaw offset to the right side (Figure 2), limitation of mouth opening, occlusion vertical dimension decrease, difficulty in pronunciation of words and to swallow, were detected during the clinical examination. It was also observed that the premolars, inferiors central and lateral incisors on both sides had great destruction. The treatment planning initially aimed to give jaw alignment in relation to the median sagittal plan and the restoration of vertical dimension of occlusion in the light of the absence of the muscles masticatory on the right side. Initially, the patient was underwented to the use of a flat and plan occlusal appliance, manufactured with colorless acrylic resin adapted to the mandibular dental arch, for reconstitute the vertical dimension [17–21].

Figure 2. Mandibular deviation to the right side, due to the removal of lateral and medial pterygoid superficial and deep masseter muscles on the same side.
The patient used the appliance for a period of thirty days, every day, removing it only for the meals. At the end of the period it was observed that the jaw was not completely aligned to the median sagittal plan, because of the removal of muscles on the right side. So a ramp was added on the appliance occlusal surface in the right side (Figure 3) direct the jaw to median sagittal plan. The alignment was got at the 60’s days of use (Figure 4).

Figure 3. Ramp built on the right side of the unit, to the alignment of the mandible in the sagittal plane.

Figure 4. Recovery of facial aesthetics after the alignment of the mandible in relation to the sagittal plane and normalization on the vertical dimension of occlusion.
The use of the appliance allowed not only the jaw alignment to the median sagittal plan, but the occlusal vertical dimension was normalized. Then the patient underwent to a preventive duodenum and stomach endoscopy and the medical report showed that the oral cavity, the oropharynx and the hypopharynx were aligned with the upper structures of the digestive system. Due to the surgical therapy for the oncological treatment, the patient had a supplementary feeding through intestinal probe.
All the mandibular teeth were underwented to an endodontic treatment to receive o’rings systems and copings (Figure 5). The roots of the mandibular canines and premolars of both sides received the o’rings systems. After the cementing of the restraint systems and copings (Figure 6) the over denture was made as usual and the technique determines the capsules with the rubber rings held routinely [1–3]. The patient was instructed to make use of pasty foods in the first 15 days and your new prostheses were submitted to weekly setting. After this period, he began to use solid foods more resilient and more fibrous gradually. The patient expressed sense of satisfaction and comfort with the use of the prosthesis (Figure 7 and 8) and reported an increase in body weight of ten kilograms and plans to the removal of the intestinal probe.

Figure 5. Mandibular teeth received short copings or ball attachment systems for overdenture o’ring type. The illustration shows the restraint systems and the copings being proven in the roots of the teeth.

Figure 6. After casting and machining procedures ball attachment systems and the copings were installed in the mouth.

Figure 7. Prosthesis adapted on restraint systems and in teeth occlusion antagonists.
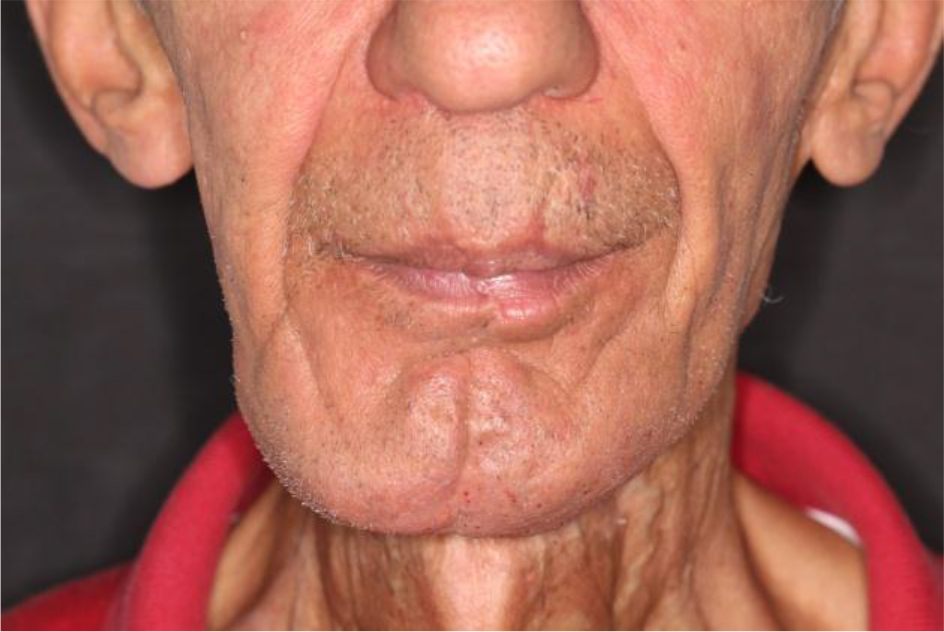
Figure 8. Facial aesthetics re-established masticatory function, within the limitations of clinical case.
Summary
Male patient undergo laryngectomy and supraglottic glossopelvemandibulectomy cervical bilateral radical emptying due to an ulcerated moderately differentiated spin cell carcinoma and invasive (degree II). Underwent successful before treatment of prosthetic rehabilitation treatment with occlusal appliance smooth and flat and later device with lateral ramp to align the mandible in relation to the median sagittal plan. The prosthetic rehabilitation occurred through mandibular overdenture with o’ring retention system. After a period of adaptation, the patient reported satisfaction and comfort and an increase in body weight of 10 kilograms.
Discussion
Surgical treatment of carcinogenic head and neck injuries often results in often severe intraoral and extraoral defects that lead to changes in chewing, swallowing, phonation and aesthetics, influencing the patient’s quality of life. As a means of restoring function and partially or totally aesthetics, prosthetic rehabilitation becomes the main recommendation for this purpose. Overdenture has been described as a technique indicated for prosthetic rehabilitation, where removal of part of the maxilla or mandible is necessary as a preventive approach to recurrence of invasive carcinomas. The o’ring system is indicated as a form of retention of overdentures whether installed on natural or artificial abutments.
The indication of implant overdenture in irradiated patients who underwent chemotherapy presents a risk of osseointegration loss and, as a consequence, impairment of the prosthesis. In these cases the use of natural teeth as o’ring system receptors are more indicated, having the advantage of maintaining dental proprioception. The concept of a physiological mandibular position, from which the vertical occlusion dimension and the maximum intercuspal position for the construction of prosthetic rehabilitation can be established, is unanimous in the dental environment. Although there are discussions regarding the procedures for obtaining such positions, the tendency of the researchers is to adopt technical procedures to first seek neuromuscular balance and then the vertical dimension of occlusion and maximum intercuspal position. It is noticed that the initial or pre-rehabilitative objective is proprioceptive block, so that the masticatory muscles and associated muscles can equalize their functions, bilaterally.
The use of a rigid, smooth and flat intraoral device that blocks proprioception and as a consequence allows the electromyographic equalization of the masticatory muscles, as a consequence brings the mandible in harmony with the position of the condyles in the mandibular fossae and the muscular electrical activity. Thus, the jaw responding to bilateral functional activity of the muscles in balance, reaches a therapeutic position, ready to receive prosthetic rehabilitation. The case described in this article was planned and executed using initially a rigid, smooth and flat intraoral device, seated on the lower teeth to initially promote muscle equalization. As it was necessary the total removal of the right mandibular ramus and all the muscles inserted in it, later, the intraoral device was transformed, receiving an inclined plane, in its right side to dislocate the mandible, towards the midline of the median sagittal plane and thus centralizing it. After stabilization of the mandible in this position, an o’ring overdenture was performed on the remaining lower teeth, in addition to functional and aesthetic rehabilitation, seeking to improve the patient’s quality of life.
References
- Burns DR (2004) The mandibular complete overdenture. Dent Clin North Am 48: 603–623. [crossref]
- Mericske-Stern R (1994) Overdentures with roots or implants for elderly patients: a comparison. J Prosthet Dent 72: 543–550. [crossref]
- Ledger E (1856) On preparing the mouth for the reception of a full set of artificial teeth. Br J Dent Sci 1: 90.
- PRINCE IB (1965) CONSERVATION OF THE SUPPORTIVE MECHANISM. J Prosthet Dent 15: 327–338. [crossref]
- Fenton AH1 (1998) The decade of overdentures: 1970–1980. J Prosthet Dent 79: 31–36. [crossref]
- Morrow RM, Powell JM, Jameson WS, Jewson CG, Rudd KD (1969) Tooth supported complete dentures: an approach to preventive prosthodontics. J Prosthet Dent 21: 513–522.
- Chrcanovic BR, Albrektsson T, Wennerberg A (2016) Dental implants in irradiated versus nonirradiated patients: A meta-analysis. Head Neck 38: 448–481. [crossref]
- Garg A, Guez G (2011) Head and neck cancer, dental implants, and dental oncology. Dent Implantol Update 22: 1–8. [crossref]
- De la Plata M, Gías LN, Díez PM, Muñoz-Guerra M, González-García R, et al. (2012) Osseointegrated implant rehabilitation of irradiated oral cancer patients. J Oral Maxillofac Surg 70: 1052–1063.
- Yerit KC, Posch M, Seemann M, Hainich S, Dörtbudak O, et al. (2006) Implant survival in mandibles of irradiated oral cancer patients. Clin Oral Implants Res 17: 337–344. [crossref]
- Marx RE, Johnson RP (1987) Studies in the radiobiology of osteoradionecrosis and their clinical significance. Oral Surg Oral Med Oral Pathol 64: 379–390. [crossref]
- Jacobsson M, Tjellström A, Thomsen P, Albrektsson T, Turesson I (1988) Integration of titanium implants in irradiated bone. Histologic and clinical study. Ann Otol Rhinol Laryngol 97: 337–340. [crossref]
- Sammartino G, Marenzi G, Cioffi I, Teté S, Mortellaro C (2011) Implant therapy in irradiated patients. J Craniofac Surg 22: 443–445. [crossref]
- Schiegnitz E, Al-Nawas B, Kämmerer PW, Grötz KA (2014) Oral rehabilitation with dental implants in irradiated patients: a meta-analysis on implant survival. Clin Oral Investig 18: 687–698.
- Zheng M, Li L, Tang Y, Liang XH (2014) How to improve the survival rate of implants after radiotherapy for head and neck cancer? J Periodontal Implant Sci 44: 2–7.
- Ihde S, Kopp S, Gundlach K, Konstantinović VS (2009) Effects of radiation therapy on craniofacial and dental implants: a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107: 56–65. [crossref]
- Casselli H, Landulpho AB, Silva WA, Silva FA (2007) Electrognatographic evaluation of rehabilitated edentulous patients. Braz Oral Res 21: 355–361.
- Landulpho AB, Silva WA, Silva FA, Vitti M (2002) The effect of the oclusal splints on the treatment of temporomandibular disorders – a computerized electromyographic study of masseter and anterior temporalis muscles. Electromyogr Clin Neurophysiol 42: 187–191.
- Landulpho AB, Silva WA, Silva FA, Vitti M (2004) Electromyographic evaliation of masseter and anterior temporalis muscles in patients with temporomandibular disorders following interocclusal appliance treatment. J Oral Rehabil 31: 95–98.
- Landulpho AP, Silva WAB, Silva FA, Casselli H, Silva LLB (2004) Electrosonographic evaluation in patients with temporomandibular disorders, treated by interoclusal appliance. Braz J Oral Sci 11: 624–627.
- Silva WAB, Silva FA (2000) Epidemiologic study of the temporomandibular disorders. J Dent Res 79: 584–588.