Abstract
Background: A number of new interventions have recently influenced mortality, once considered an incurable disease. Manual therapy, specifically manipulation, has the potential to be an influential intervention.
Study Design: This case report was created using CARE guidelines. A case report is a narrative that describes, for medical, scientific, or educational purposes, a medical problem experienced by one or more patients. In this example, a patient was seen for one visit, followed by a dedicated home exercise program. The patient received a repeated measures spinal manipulation that was designed to improve mobility, morbidity and mortality. Notable significant changes were seen after care.
Discussion: Overall improvements were notable but the study design does not permit causality or does it allow us to determine if the findings are clinically significant. A randomized controlled trial may improve the generalizability of findings.
Keywords
Spinal manipulation, repeated measures, Gouda, Death
Introduction
Worldwide, annually, there are 55.3 million people who die [1]. Although the reasons for death may vary from country to country, the most common causes of mortality (death) include: 1) Lung, Tracheal, and Bronchial Cancers (1.6 million deaths, 3.0% of all deaths), 2) Chronic Obstructive Pulmonary Disease, (3.17 million deaths, 5.6% of all deaths), 3) Lower Respiratory Infections (3.19 million deaths, 5.6% of all deaths), 4) Stroke (6.2 million deaths, 11.1% of total deaths), and 5) Ischemic Heart Disease (8.7 million deaths, 15.5% of total deaths) [2]. In 2010, the World Health Organization [3] sponsored an initiative to reduce mortality rates in the world to 0% by 2025. This lofty initiative occurred concurrently with a request for study involving interventional methods to reduce deaths in humans.
Past research has indicated that mortality is a fugue-like state, generally characterized with low health reported outcomes [4]. Mortality has been shown to reduce work productivity, increase the risk of decreased activity, and lower one’s socialization. Previous interventions such as surgery, Reiki, and cognitive behavioral therapy have only shown limited rates of effectiveness on mortality [5]. To date, manual therapy, which is characterized by lymphatic drainage, craniosacral, manual traction, massage, mobilization/ manipulation, and passive range of motion, has not been tested for reducing mortality rates [6]. Past studies have suggested that manual therapy is effective in the treatment of deafness, osteoarthritis, colic, cancer, autism, and chronic halitosis [7]. Therefore, the purpose of this case report is to describe the temporal effects of manual therapy, specifically spinal manipulation, on a deceased patient with a spinal cord injury.
Methods
Guidelines
Reporting of this manuscript was created using the CARE guidelines [8]. The CARE guidelines for case reports help reduce bias, increase transparency, and provide early signals of what works, for which patients, and under which circumstances [8]. To further improve reporting standards, we also followed the PRISMA guidelines [9], the TSA guidelines for traveling with fluids [10], and the CONSORT guidelines [11].
Clinical History and Physical Examination
The patient in this case was a 26-year-old male who was recently employed as a Barista. At the time of the treatment, the patient no longer worked. All vital signs were absent. He was right hand dominant. At the initial assessment, his family members reported that he had exhibited markedly decreased activity, little interest in socialization, and “tended to lay around all day”. The patient had previously received 10 sessions of physical therapy consisting of deep and painful massage to the forearm muscles, ice therapy, laser, cognitive behavioral therapy, postural restoration, and sensory electrical stimulation. An exercise program was also prescribed, but at the time of the treatment, the patient was no longer exercising. Since the patient experienced little progress since the onset of the condition, his family members sought assistance from another therapist (hence the new treatment). A period of approximately 5 years elapsed from the previous treatment period and the time the patient entered our clinic. At the time of the treatment associated with this case report, rest did not seem to be assisting the patient.
Patient History and Outcomes Measures
A detailed patient history was deferred. Patient reported outcomes measures were used to assess the health morbidity and quality of life. At baseline, the patient scored a 0 for his SF-12 MCS and PCS score [12], suggesting very poor quality of life. His Oswestry disability index score was 100 [13], suggesting a high degree of disability. We also used a Timed Get up and Go test [14] and the patient’s score was infinite, as he was unable to rise from the chair. The pain-free grip force (PFG) [15] was also included in the functional analysis. For that purpose, a hydraulic dynamometer (Enterprises Inc, Irvington, NY, USA) was used. PFG was calculated with the upper extremity in a standard position of elbow extension and forearm pronation. The patient was instructed to grip the dynamometer until the pain was first provoked. The mean grip strength was 0. (Table 1) outlines the values of his initial examination. A perceived improvement of our patient at the end of visit one and at four months follow-up periods was assessed with a Global Rating of Change (GROC) on a 15-point Likert scale ranging from -7 (a very great deal worse) to +7 (a very great deal better) [16]. Descriptors of perceived worsening or improving were assigned with values ranging from -1 to -7 and +1 to +7, respectively [17].
Table 1. Disability, Function, and Grip Strength Values at Initial Visit.
|
Assessment |
Mean Score (SD) |
Comments |
|
SF-12 MCS and PCS |
0 (0) and 0 (0) |
Quality of life was presumably low |
|
Oswestry Disability |
100 (16.3) |
Although little pain was expressed, the patient demonstrated very low mobility |
|
Timed up and Go |
Inf |
The patient was unable to initiate rising from the chair |
|
Grip Strength (in kilograms) |
0 (0) |
Surprisingly, the grip strength was very low. In full disclosure the patient seemed inattentive when we requested the three repetitions |
Clinical Reasoning
Due to the patient’s very low levels of function and high levels of morbidity, it was decided that the previous treatment was not effective and that he was not doing very well. The treating clinician and one of the authors of this paper, then determined that a manual therapy intervention was appropriate for his current state. His reduced overall mobility increased his likelihood for a spinal manipulation [18]. Also, he met two clinical prediction rules [19], he had high treatment expectations [20] and low fear avoidance [21], and he centralized during repeated movements [22]. Most importantly, he has subluxations all over his body [23], which were evident using a diagnostic ultrasound [24]. Based on experience, the treating therapist was convinced that only one session of spinal manipulation was needed.
Spinal Manipulation Procedure
After the application of rubbing alcohol, the patient received the spinal manipulation (see Figure 1) [25]. The technique has been previously described in the literature [26]. This technique is performed as follows: one hand of the therapist is used to compress the pelvis while the other hand is used to rotate the thoracic spine away from the pelvis. The technique usually leads to a cavitation [25]. In our case report, a Belt® was not used, nor was there the need for several assistants to hold the patient during the procedure. Two hundred and fifty repetitions were performed with an approximate 15-second rest interval between repetitions [26]. Feedback was solicited by the clinician after each repetition and recorded.

Figure 1. Manipulation Method used in Case Report.
Home exercise
The family was instructed to perform the same procedure at home, using the same two hundred fifty repetition interval process. Because of the intense nature of the intervention, immediate, first and second cousins and all next of kin were solicited. Based on previous care guidelines, they were instructed to perform the treatment hourly [27].
Results
Initially, the repeated spinal manipulation procedure appeared to have little value. At manipulation 176, the patient reported a decreased ODI score of 21/100. By manipulation 250, the ODI has dropped to 6/100 (an overall 3% improvement). The SF12 score also improved. After manipulation 250, the SF12 improved to 45 (SD-47) whereas the MCS also improved by less robustly to 34 (SD=18). Timed up and Go reduced form the infinite score obtained earlier in the visit to a score of 18 seconds; an increase of 12% from baseline. His grip strength increased to 14 kilotons of force, a notable 2.3% change from baseline. The GRoC score was -2, suggesting that the patient did not experience a meaningful change. (Table 2) Represents the changes over the single temporal session. (Figure 2) demonstrates the temporal change across the 250 spinal manipulations. Of particular interest is the rising squared lines and it’s interaction with the rising triangle lines. This suggests that the outcomes were related to one another and that no single measure was superior. Further, the “major” tick was the first notable “response” by the patient.
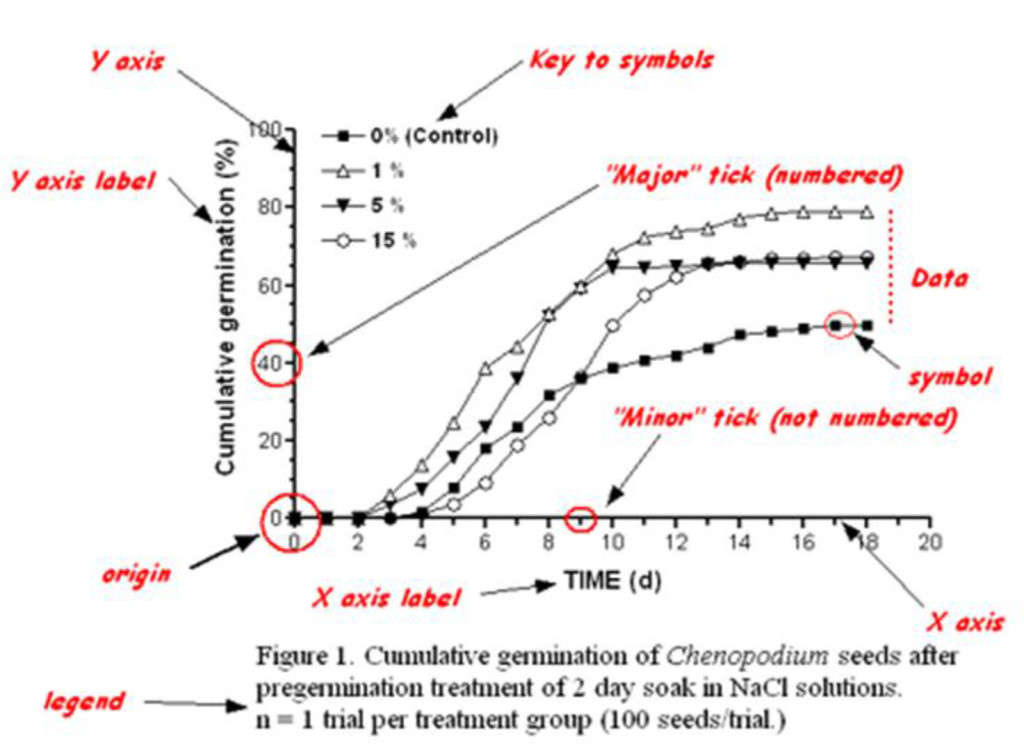
Figure 2. Changes in Outcomes during 250 Repetition Manipulation.
Table 2. Disability, Function, and Grip Strength Values after First Visit.
|
Assessment |
Mean Score (SD) at Baseline |
Mean Score (SD) after 250 Manipulations |
P value |
|
SF-12 MCS and PCS |
0 (0) and 0 (0) |
45 and 34 |
0.03 |
|
Oswestry Disability |
100 (16.3) |
6 (17.4) |
<0.01 |
|
Timed up and Go |
Inf |
18 seconds |
<0.01 |
|
Grip Strength (in kilotons) |
0 (0) |
14 (N/A) |
0.37 |
Follow up at 4 months exhibited similar findings. (Figure 3) reflects the longitudinal trend analysis of outcomes exhibited by the patient. The family reported that they discontinued the 250 spinal manipulations each hour after 1.5 months as it seemed that the procedure had “flat lined”. Qualitatively, the family members have reported that the patient is more active, his color was better, he socialized more, and “did not lay around as much”. At the time of the follow-up he had not returned to his prior work as a barista but was considering work in the movie industry.

Figure 3. Longitudinal Trend Analysis of Outcomes.
Discussion
This case report describes the careful use of a spinal manipulation to reduce mortality in a 26-year-old male. Whereas this case study does not assume causality, the findings are interesting enough to report and discuss. We are most intrigued with the improvement in the timed up and go findings, as these suggest that the patient only lacks some speed to cross the road in Boston [28]. The improved handgrip strength findings are likely related to his improved diet [29]. Socrates once said; “death may be the greatest of all human blessings.” Khalil Gibron has responded by saying “as life and death are one, the river and the sea are one”. Neither of these two quotes have any relevance to our case. Responding to both individuals (Socrates and Gibron), we would argue that mortality is a reversible condition that may be amenable to spinal manipulation. We would argue that more study is needed, especially another systematic review from Sydney Australia [30]. We are concerned that the SF-12 MCS scores did not improve at the rate that the SF-12 PCS improved. This suggests that the patient was still harboring some cognitive-emotional concerns about his prior mortality [31]. We are certain that the patient was catastrophizing about his prior mortality, although we did not measure this. One option we could have considered was “explaining pain” to our patient. Explaining pain and suggesting the condition is completely within the head of the patient has been shown to cure every condition that is musculoskeletal in nature [32]. Dumbed down versions of Explain Pain are all the rage now and our treatment was very focused on trendy topics with marginal evidence. With better training on the clinician’s side, explaining the patient’s situation to him may reduce his concerns. It is worth reporting that the patient did exhibit a notable change in condition but we are not willing to assume that his change is clinically meaningful [33]. In order to have a clinically meaningful change, the patient would have had to score a 5 out of 7 on the GRoC [34]. Indeed, his change scores could reflect natural history and a randomized controlled trial is needed to verify treatment effectiveness. Further, the patient reported a -2 on his GRoC, suggesting he, himself, did not find the change meaningful. [35] Past individuals who were full of subluxations have also reported similar findings.
Limitations
In the original clinical trial, a pragmatic approach was utilized for the treatment of the lumbar spine in both groups. The exercise program for the LBP plus hip group in the original trial may have had some potential crossover and impact the strength of the trunk musculature. The pragmatic nature of the interventions could have led to wide variation in treatments rendered. In addition, all of the treating therapists had advanced manual therapy training and loss of clinical equipoise, thus may have provided a greater emphasis on the manual therapy techniques during the treatment sessions, which may not reflect typical clinical practice.
Conclusion
This case report describes the careful use of a spinal manipulation to reduce mortality in a 26-year-old male. Whereas this case study does not assume causality, the findings were interesting enough to report and discuss. Future studies such as randomized controlled trials should be used for causality.
References
- World Birth and Death Rates; Accessed on August 15th, 2018 at: http://www.ecology.com/birth-death-rates/.
- Top Ten Leading Causes of Death In The World. Access on August 15th, 2018 at: https: //www.worldatlas.com/articles/top-ten-leading-causes-of-death-in-the-world.html.
- Outbreaks, behind the headlines/ Accessed on August 15th, 2018 at: http://www.who.int/.
- Whedon JM, Toler AWJ, Goehl JM, Kazal LA (2018) Association Between Utilization of Chiropractic Services for Treatment of Low Back Pain and Risk of Adverse Drug Events. J Manipulative Physiol Ther. 41: 383–388. [crossref]
- Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, et al. (2015) The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg 78: 306–311. [crossref]
- Johnson CC, Long T (2009) Use of the Guide to Physical Therapist Practice by pediatric physical therapists. Pediatr Phys Ther 21: 176–186. [crossref]
- Barrett S (2018) Evidence of Unscientific Teachings at Canadian Memorial Chiropractic College. Accessed on August 15th, 2018 at: https: //www.chirobase.org/03Edu/york.html
- Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, et al. (2014) The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol 67: 46–51.
- Ioannidis JPA, Stuart ME, et al. (2017) How to survive the medical misinformation mess. Eur J Clin Invest 47: 795–802. [crossref]
- Schwartz D, Lellouch J (2009) Explanatory and pragmatic attitudes in therapeutical trials. J Clin Epidemiol 62: 499–505. [crossref]
- Cooper NA, Scavo KM, Strickland KJ, Tipayamongkol N, et al. (2016) Prevalence of gluteus medius weakness in people with chronic low back pain compared to healthy controls. Eur Spine J 25: 1258–1265. [crossref]
- Kankaanpää M, Taimela S, Laaksonen D, Hänninen O, Airaksinen O (1998) Back and hip extensor fatigability in chronic low back pain patients and controls. Arch Phys Med Rehabil 79: 412–417. [crossref]
- Nadler SF, Malanga GA, DePr ince M, Stitik TP, Feinberg JH (2000) The rela-tionship between lower extremity injury, low back pain, and hipmuscle strength in male and female collegiate athletes. Clin J SportMed 10: 89–97. [crossref]
- Nadler SF, Malanga GA, Feinberg JH, Prybicien M, Stitik TP, et al. (2001) Relationship between hip muscle imbalance and occurrence of lowback pain in collegiate athletes: a prospective study. Am J Phys MedRehabil 80: 572–577. [crossref]
- Nadler SF, Malanga GA, Bartoli LA, Feinberg JH, Prybicien M, et al. (2002) Hip muscle imbalance and low back pain in athletes: influence of core strengthening. Med Sci Sports Exerc 34: 9–16. [crossref]
- Selkowitz DM, Beneck GJ, Powers CM (2013) Which exercises target the glu-teal muscles while minimizing activation of the tensor fascia lata? Electromyographic assessment using fine-wire electrodes. J OrthopSports Phys Ther 43: 54–64. [crossref]
- Hando BR, Gill NW, Walker MJ, Garber M (2012) Short- and long-termclinical outcomes following a standardized protocol of orthopedicmanual physical therapy and exercise in individuals with osteoar-thritis of the hip: a case series. J Man Manip Ther 20: 192–200. [crossref]
- Hengeveld E (2013) Maitland’s Peripheral Manipulation: Management of Neuromusculoskeletal Disorders. 5th ed. 2 Edinburgh: Churchill Livingstone; 616 pg: 34.
- Fritz JM, Irrgang JJ (2001) A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther 81: 776–788. [crossref]
- Abedin T, Al Mamun M, Lasker MAA, Ahmed SW, Shommu N, et al. (2017) Social Media as a Platform for Information About Diabetes Foot Care: A Study of Facebook Groups. Can J Diabetes 41: 97–101. [crossref]
- Ahmed OH, Weiler R, Schneiders AG, McCrory P, Sullivan SJ (2015) Top tips for social media use in sports and exercise medicine: doing the right thing in the digital age. Br J Sports Med 49: 909–910. [crossref]
- Allcott H, Gentzhow M (2017) Social media and fake news in the 2016 election. Journal of Economic Perspectives 31: 211–236. http://dx.doi.org/10.1257/jep.31.2.211.
- Bercovici J. Who coined ‘social media’? Web pioneers compete for credit. Forbes. December 9, 2010. Accessed July 12, 2017. https://www.forbes.com/sites/jeffbercovici/2010/12/09/who-coined-social-media-web-pioneers-compete-for-credit/#28ed6ece51d5.
- Berry D. Social media spaces. Darrell Berry / Social Media Spaces Web site. http://www.ku24.com/~darrell/hybrid1.html. Published October 19, 1995. Accessed July 12, 2017.
- Boutron I, Dutton S, Ravaud P, Altman DG (2010) Reporting and interpretation of randomized controlled trials with statistically nonsignificant results for primary outcomes. JAMA 303: 2058–2064. http://dx.doi.org/10.1001/jama.2010.651
- Brynolf A, Johansson S, Appelgren E, Lynoe N, Edstedt Bonamy AK (2013) Virtual colleagues, virtually colleagues—physicians’ use of Twitter: a population-based observational study. BMJ Open 3: e002988. http://dx.doi.org/10.1136/bmjopen-2013–002988
- Budd L, Fidler L, Anand A (2016) Gaining competence through social media. CMAJ 188: 311–312. [crossref]
- Chambers C. Centre for Pediatric Pain Research. It Doesn’t Have to Hurt: Proven Pain Control for Children Web site. http://itdoesnthavetohurt.ca. Published 2015. Accessed July 21, 2017.
- Choo EK, Ranney ML, Chan TM, Trueger NS, Walsh AE, et al. (2015) Twitter as a tool for communication and knowledge exchange in academic medicine: A guide for skeptics and novices. Med Teach 37: 411–416. [crossref]
- Djuricich AM (2014) Social media, evidence-based tweeting, and JCEHP. J Contin Educ Health Prof 34: 202–204. [crossref]
- Evaniew N, Adili AF, Ghert M, et al. (2017) The scholarly influence of orthopaedic research according to conventional and alternative metrics: a systematic review. JBJS Rev. 5: e5. http://dx.doi.org/10.2106/JBJS.RVW.16.00059
- Eysenbach G (2011) Can tweets predict citations? Metrics of social impact based on Twitter and correlation with traditional metrics of scientific impact. J Med Internet Res 13: e123. http://dx.doi.org/10.2196/jmir.2012
- Gewandter JS, McKeown A, McDermott MP, et al. (2015) Data interpretation in analgesic clinical trials with statistically nonsignificant primary analyses: an ACTTION systematic review. J Pain.; 16: 3–10. http://dx.doi.org/10.1016/j.jpain.2014.10.003
- Gottfried J, Shearer E. News use across social media platforms 2016. Pew Research Center Web site. http://www.journalism.org/2016/05/26/news-use-across-social-media-platforms-2016/. Published May 26, 2016. Accessed July 21, 2017. http://dx.doi.org/10.1016/j.jpain.2014.10.003
- Grande D, Gollust SE, Pany M, et al. (2014) Translating research for health policy: researchers’ perceptions and use of social media. Health Aff (Millwood) 33: 1278–85. http://dx.doi.org/10.1377/hlthaff.2014.0300