Abstract
Several techniques have been introduced to improve the success rate and efficiency of the ProsealTM laryngeal mask airway (PLMA) placement along with decreasing complication. The aim of this study is to compare the success rate of the nasogastric catheter guided technique to the conventional digital technique.
Methods
In this randomized-controlled clinical trial, 200 patients, age between 18 and 65 years old, underwent inhalation technique anesthesia were enrolled. Participants were randomized by computer to Nasogastric catheter guided group (NG) and Digital technique group (DT). Anesthesia was induced with propofol (3 mg/kg) and fentanyl (2 mcg/kg). In DT group, the PLMA was inserted by using the index finger insertion technique. In NG group, PLMA with nasogastric catheter protruding for 5 cm from the PLMA drain tube distal aperture was inserted with the same method. Successful insertion was evaluated by the chest movement and the persistent rising of end-tidal carbon dioxide. The quality of placement was also recorded after the patient regained spontaneous breathing. Complications were evaluated at the end of the surgery and at the PACU discharge time.
Result
Patient characteristics were similar in both groups. The overall insertion success rates were similar; 89.3% in NG and 81.5% in DT group (P=0.22). There was no difference in insertion attempt (success rate in the first attempt = 86.7% and 84.0% in NG group and DT group respectively, P = 1.00). The time to the success of insertion was not significantly different; 30 seconds in NG group vs 35 seconds in DT group (P=0.185). There were no differences in the complications such as airway bleeding, sore throat, dysphagia, and hoarseness.
Conclusion
Insertion of Proseal LMA using nasogastric catheter guided technique did not provide an advantage over digital technique. The complications from both insertion techniques were also similar.
Keywords
Proseal LMA, Nasogastric catheter, Airway device
Background
Laryngeal mask airway (LMA) is an alternative airway device widely used during elective surgical procedures. ProsealTM LMA (PLMA) is another advanced form of this supraglottic airway device. PLMA may be inserted by the standard index finger or by using the introducer. Several techniques have also been introduced to improve the success rate and efficiency of the PLMA placement along with decreasing the complications [1,2] [4–8] [10].
The previous studies comparing the success rate of PLMA insertion showed that the use of suction catheter guided insertion had the higher success rate than the insertion without the guide [1,2]. Gum elastic bougie (GEB) guided insertion was not different in comparison to the metallic introducer in the point of success rate but it showed the improvement of the position of PLMA placement [3]. Using laryngoscope to direct insertion of GEB into esophagus before assisting PLMA insertion further improved the success rate significantly [4–6]. However, the mucosal trauma occurrence was higher with GEB guided insertion. Flexi-slip stylet guided insertion also showed higher success rate together with decreasing trauma complications [7]. The airway stylet; Foley airway stylet (FAST), had similar outcomes but it had the higher trauma rate compared to the metallic introducer [9]. Additionally, neuromuscular blocking agents could be used to improve the laryngeal airway insertion [11]. Advancing the guide such as the suction catheter into esophagus 10 to 15 centimeters to guide PLMA had the higher success rate as well [8–10].
Methods
This randomized controlled clinical trial was approved by the Ethics Committee of the Faculty of Medicine, Prince of Songkla University (ethical number: 59-192-08-1). Data were collected from October 2016 to October 2017. We recruited 200 patients, with the age between 18 – 65 years old, the American Society Anesthesiologists physical status I – III, who underwent inhalation technique of anesthesia. Patients who had body weight lower than 30 kilograms or heavier than 70 kilograms or body mass index more than 35 kilograms per square centimeters, history or suspicion of difficulty in airway management, the risk of aspiration, respiratory diseases and change of anesthetic technique were excluded from the study. Computerized randomization was performed to divide participants into nasogastric catheter guided technique group (NG) and Digital technique group (DT) equally. The opaque envelopes containing group assignment were opened prior to the start of the induction of anesthesia.
The patients were not given sedative agents for premedication. The patient position was supine without the pillow. After applying the standard monitoring and preoxygenation for 3 minutes with 100% oxygen, anesthesia was induced with propofol (3 mg/kg) and fentanyl (2 mcg/kg) intravenously. Additional boluses of propofol 0.5 mg/kg intravenously were given as required to achieve the adequate depth of anesthesia, apnea, and adequate jaw relaxation. The PLMA insertion was performed by the first or second-year anesthetic residents or in-training anesthetic nurses who had experience more than 5 success of LMA insertion. In DT group, the PLMA was inserted by using index finger insertion technique according to the manufacturer’s instruction manual. In NG group, PLMA with nasogastric catheter protruding for 5 cm from the PLMA drain tube distal aperture was inserted with the same method. The PLMA size 3 or 4 selection was based on anesthesiologists’ consideration. Neuromuscular blocking agents were not allowed to be used. The duration for insertion started as the opening of the patient’s mouth and ended after successful insertion proved by chest movement along with the ventilation and the persistent rising of end-tidal carbon dioxide for at least 5 waves. If unsuccessful insertion occurred, PLMA would be removed, then preoxygenation and additional propofol bolus doses were provided. PLMA insertions were allowed for only 2 attempts, after that, it was considered as failed insertion then the airway management was followed by the discretion of anesthetic staff. In both groups, the PLMA cuff was inflated with air to the pressure of 40 centimeters of water. Patient’s ventilation was assisted until regaining of the spontaneous breathing. Anesthesia was maintained with volatile anesthetic agent and 50% of oxygen in air. Five minutes later, the secondary outcomes were assessed by following; the position of the nasogastric catheter placement confirmed with the audible sound at epigastrium by 10 milliliters of air push, hypercapnia (End tidal Carbon dioxide more than 60 mmHg), hypoxia (Oxygen saturation less than 95%) and the leakage of ventilation (leakage sound through the patient’s mouth). The awake technique for PLMA removal was used at the end of anesthesia.
The complications were assessed after removal of PLMA. Any visible blood stain or blood in the early oropharyngeal secretion suction was noted. Patients were asked for the sore throat, hoarseness or dysphagia before discharging from PACU by PACU nurses who were blinded to the insertion technique.
Statistical analysis
The sample size was calculated from the difference of the success rates in the previous study [1]. The number of population required for this study was 90 patients for each group. With the 10% drop-out rate, therefore, the definite number of the population was 100 patients in each group. This estimation would give a power of 80% to detect the difference at the significance level of 0.05.
Statistical analysis was performed using R software. Continuous variables were presented as median and interquartile range (IQR) or mean. Categorical variables were presented as number of patients and percentages. Continuous variables were analyzed by Student t-test or Wilcoxon Rank Sum test. Categorical variables were analyzed by Fisher’s exact test, or Chi-square test. P value less than 0.05 was considered as statistical significance.
Result
Two hundred participants were enrolled into the study, eight patients in DT group and sixteen patients in NG group were excluded (Figure 1). Patient characteristics were not significantly different (Table 1).
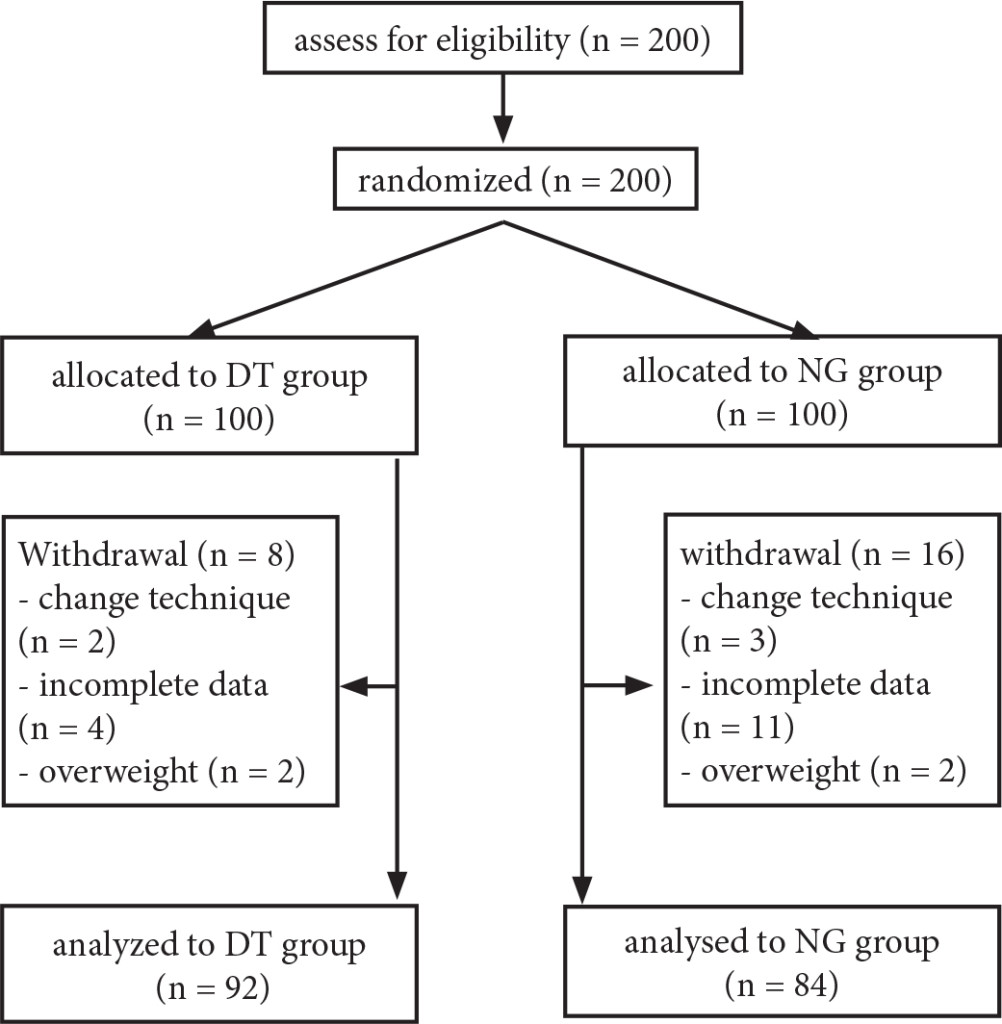
Figure 1. Consort flow diagram
Table 1. Demographic data of the patients.
|
|
NG (n=84) |
DT (n=92) |
P-value |
|
Age (year)* Gender+ – Male – Female |
45 (32–51)
16 (19) 68 (81) |
46 (35–54)
24 (26) 68 (74) |
0.20 0.35 |
|
Weight (kg)* |
58 (49–65) |
60 (52–63) |
0.56 |
|
Height (cm)* |
157 (154–160) |
158 (154–165) |
0.41 |
|
BMI• |
22.8 (3.0) |
22.8 (3.5) |
0.89 |
|
ASA+ – I – II – III Mallampati score+ – I – II – III Proseal size – 3 – 4 Performer – In-training anesthetic nurse – 1st year resident – 2nd year resident |
20 (23.8) 64 (76.2) 0 (0)
36 (42.9) 44 (52.4) 4 (4.8)
36 (42.9) 48 (57.1)
39 (46.4) 29 (34.5) 16 (19) |
22 (23.9) 68 (73.9) 2 (2.2)
48 (52.2) 42 (45.7) 3 (2.2)
32 (34.8) 60 (65.2)
51 (55.4) 29 (31.5) 12 (13) |
0.60
0.38
0.35
0.40
|
* Data are presented as a median (IQR)
+ Data are presented as a number (%)
• Data are presented as a mean (SD)
There were no significant difference in success rates (Table 2). Success rate in NG group at first attempt was 86.7% and 13.3% in second attempt. In DT group, success rate at first attempt was 84% and 16% in second attempt. The overall success rate were 89.3% in NG group and 81.5% in DT group (P value = 0.216). By the Logistic regression analysis with the insertion success as the outcome variable, there was no significant variables (ASA status, Mallampati score, the performers, PLMA size).
Table 2. Success and quality of PLMA placement
|
|
NG |
DT |
P-value |
|
Insertion success+ Insertion attempt+ – 1 – 2 |
75 (89.3)
65 (86.7) 10 (13.3) |
75 (81.5)
63 (84.0) 12 (16.0) |
0.22 0.82 |
|
Insertion time (second)* |
30 (25–47) |
35 (25–54) |
0.38 |
|
Proper nasogastric catheter placement+ |
68 (90.7) |
60 (80.0) |
0.11 |
|
Hypoxemia+ |
2 (2.7) |
3 (4.0) |
1.00 |
|
Hypercapnia+ Leakage+ |
2 (2.7) 32 (42.7) |
2 (2.7) 29 (38.7) |
1.00 0.74 |
* Data are presented as a median (IQR)
+ Data are presented as a number (%)
• Data are presented as a mean (SD
For the success of PLMA insertion (75 cases) in both groups, there were no differences in the time to success insertion and the PLMA position. The duration of insertion were 30 seconds (IQR = 25 – 47 seconds) in NG group and 35 seconds (IQR = 25 – 54 seconds) in DT group. The nasogastric catheter placement in the proper position were not significantly different which were 68 of 75 (90.7%) patients in NG group and 60 of 75 (80%) patients in DT group. The incidences of hypoxemia, hypercapnia and air leakage were not significant difference.
The visible blood stain on PLMA or in the early suction was noted after PLMA removal. Bleeding was found similarly both in NG group (24%) and in DT group (20%) (P-value = 0.693). Sore throat was reported by 36% of patients in DT group and 26.7% of patients in NG group (P-value = 0.291). Dysphagia was the same as 4% in both groups (Table 3). Hoarseness was not significantly different between the two groups (4% and 2.7% in NG and DT groups, respectively). The symptoms of all patients improved within two days postoperatively.
Table 3. Airway complications
|
|
NG |
DT |
P-value |
|
Bleeding Sore throat |
18 (24) 20 (27) |
15 (20) 27 (36) |
0.69 0.29 |
|
Dysphagia Hoarseness |
3 (4) 3 (4) |
3 (4) 2 (3) |
1.00 1.00 |
Data are presented as a number (%)
Discussion
The success rate of PLMA insertion by using the nasogastric catheter guiding was slightly higher, but not significantly different from the conventional digital technique. Due to the number of the patients in the NG group were withdrawn more than 10% drop-out, therefore, the sensitivity analysis was also performed and analyzed. The result still showed no significantly different in the success rates between the two groups. The numbers of insertion and the duration of PLMA placement were also similar between the two groups. The quality of PLMA position which determined by the proper position of the nasogastric catheter placement, hypercapnia, hypoxia and the leakage of ventilation also revealed the insignificant differences between the two groups. However, the rate of proper nasogastric-catheter-positioning was slightly higher in NG group.
The nasogastric catheter used as a guide for PLMA insertion in our hospital might be different from previous literatures. The nasogastric catheter from the different company might differ in the consistency of the material. Therefore, it might not be helpful to be the guide of the PLMA insertion in this study. Even though, the complications such as airway trauma were not significantly different. Five centimeters protrusion of nasogastric catheter from the distal end of PLMA drainage tube in our study was less than those in the previous reports so it could be inserted together with PLMA and the protruding nasogastric catheter would act as the guide to the proper positioning of PLMA. Unlike the previous studies, the nasogastric catheter was inserted 10 to 15 centimeters deep into the esophagus and then following by the PLMA [8,10]. With the longer length of nasogastric catheter, it was easier to be folded or kinked while passing through posterior pharyngeal wall causing the impediment of the PLMA insertion and also caused mucosal trauma and increased the time of insertion. In this study, the success rates were not different from the other reports (90%) in NG guided technique which also performed by inexperienced performers [1,2], whereas the success rate of the digital technique in this study was higher than those in the previous reports [1,2].
The experience of the anesthesiologist is another important factor for the successful insertion of PLMA. In the experienced hands, the success rate might not be different because of the ease of the LMA insertion by itself. In the other hand, the different techniques of insertion might affect the success in the learners. Thus, the first and second-year anesthetic residents and in-training anesthetic nurses were designed as the performers. However, the result showed no significant difference in the success rates between the two groups.
For the patients who failed PLMA insertion, half of them were managed by intubation with oroendotracheal tube. Three patients were successfully inserted the PLMA by anesthetic staff in the third attempt. However, it had to reduce the size 4 to size 3 of PLMA to achieve the successful PLMA insertion in three patients.
In DT group, there were some patients failed to properly advance the nasogastric catheter to the stomach. The cause probably be due to the misplacement of the tip of drainage tube of PLMA which was not properly at the esophageal opening or the minor folding of the tip of PLMA after insertion.
The Use of larygeal mask airway in an elective surgery is safe and has low incidences of the serious complications. The mild, short-lasting complications such as airway bleeding/trauma, sore throat, hoarseness are more common. The incidences of airway trauma and sore throat varied from 9 – 22% and 5.8 – 34% depending on the PLMA insertion techniques [11]. The complications of PLMA insertion in our study were not different from the previous studies [1,8,11] but the incidences were higher than those in the reports using laryngoscope and oesophageal vent to guide the PLMA insertion [4,12].
Limitation
First, fourteen patients were excluded from the study due to incomplete data. Even this did not affect to the primary outcome which tested by sensitivity analysis, but it might affect some other secondary outcomes. Secondly, the variation in the experience among the 13 anesthetic nurses and 17 anesthetic residents to perform PLMA insertion during the 1-year duration of the study. Thirdly, we did not use flexible fiberoptic laryngoscope to determine the proper position of placement. The malposition rate might be higher compared to the clinical judgement. Lastly, this study could not be blinded for the assessment of PLMA insertion.
Conclusion
Insertion of the Proseal LMA using nasogastric catheter protruding 5 cm from the drainage tube distal aperture for guiding technique did not provide an advantage over the index finger technique by the inexperienced performers. The complications from both insertion techniques were also similar.
Thai Clinical Trial Registry number: TCTR20161026001
Financial support of the work: Songklanagarind Hospital, Department of Anesthesia, Faculty of Medicine, Prince of Songkla University, Thailand
Conflict of Interest: none
Acknowledgement: none
References:
- Perilli V, Aceto P, Sacco T, Martella N, Cazzato MT, Sollazzi L (2014) Suction catheter guided insertion of ProSeal laryngeal mask airway: Experience by untrained physicians. Indian J Anaesth. 58(1): 25–9. [Crossref]
- Nagata T, Kishi Y, Tanigami H, Hiuge Y, Sonoda S, Ohashi Y, et al. (2012) Oral gastric tube-guided insertion of the ProSeal™ laryngeal mask is an easy and noninvasive method for less experienced users. J Anesth 26(4): 531–5. [Crossref]
- El Beheiry H, Wong J, Nair G, Chinnappa V, Arora G, Morales E, et al. (2009) Improved esophageal patency when inserting the ProSealTM laryngeal mask airway with an EschmannTM tracheal tube Introducer. Can J Anaesth 56(10): 725–32. [Crossref]
- Eschertzhuber S, Brimacombe J, Hohlrieder M, Stadlbauer KH, Keller C (2008) Gum Elastic Bougie-guided insertion of the ProSeal Laryngeal mask airway is superior to the digital and introducer tool techniques in patients with simulated difficult laryngoscopy using a rigid neck collar. Anesth Analg 107(4): 1253–6. [Crossref]
- Howath A, Brimacombe J, Keller C (2002) Gum-elastic bougie-guided insertion of the ProSeal laryngeal mask airway: a new technique. Anaesth Intensive Care 30(5): 624–7. [Crossref]
- Brimacombe J, Keller C. (2004) Gum elastic bougie-guided insertion of the ProSeal Laryngeal Mask Airway. Anaesth Intensive Care 32(5): 681–4. [Crossref]
- Chen HS, Yang SC, Chien CF, Spielberger J, Hung KC, Chung KC (2011) Insertion of the ProSealTM laryngeal mask airway is more successful with the Flexi-SlipTM stylet than with the introducer. Can J Anesth 58(7): 617–23. [Crossref]
- García-Aguado R, Viñoles J, Brimacombe J, Vivó M, López-Estudillo R, Ayala G (2006) Suction catheter guided insertion of the ProSealTM laryngeal mask airway is superior to the digital technique. Can J Anesth 53(4): 398–403. [Crossref]
- Chen MK, Hsu HT, Lu IC Shih CK, Shen YC, Tseng KY, et al. (2014) Techniques for the insertion of the proseal laryngeal mask airway: comparison of the foley airway stylet tool with the introducer tool in a prospective, randomized study. BMC Anesthesiol 14: 105. [Crossref]
- Gasteiger L, Brimacombe J, Perkhofer D, Kaufmann M, Keller C (2010) Comparison of guided insertion of the LMA ProSealTM vs the i-gelTM. Anaesthesia 65(9): 913–6. [Crossref]
- Michalek P, Donaldson W, Vobrubova E, Hakl M (2015) Complications associated with the use of supraglottic airway devices in perioperative medicine. Biomed Res Int 2015: 746560.
- Eschertzhuber S, Brimacombe J, Hohlrieder M, Keller C (2009) The Laryngeal Mask Airway SupremeTM – a single use laryngeal mask airway with an oesophageal vent: a randomized, cross-over study with the Laryngeal Mask Airway ProSealTM in paralysed, anesthetized patients. Anaesthesia 64(1): 79–83. [Crossref]