Fascial Dysfunction
Fascial degeneration can be caused by various factors (Table 1). Injury, disuse, lack of exercise due to circulatory failure, repetitive movement, and persistent poor posture can cause twisting of collagen fiber bundles and densification of the fascia, eventually leading to dehydration, hardening, and gelation of the fascial matrix. Aggregation of hyaluronic acid due to overuse and sustained muscle contraction can also limit myofascial gliding [1–3]. Generally, fascial dysfunction is caused by 1) densification of the fascia, 2) gelation of the fascial matrix, and 3) aggregation of hyaluronic acid. Fascial dysfunction reduces the gliding property and mobility of the fascia and all underlying tissues such as muscles, thereby limiting the maintenance of antigravity posture as well as smooth, functional, and efficient movements. Fascia is composed of the superficial fascia, deep fascia (aponeurotic fascia), epimysium, perimysium, and endomysium (Figure 1). The superficial fascia is in the subcutaneous tissue while the deep fascia covers muscles and connects the whole body in 14 different arrangements. The epimysium is a thin membrane that covers muscles; it connects to the perimysium to cover muscle bundles and to the endomysium to cover muscle fibers. Muscle fibers enter from the epimysium into the deep fascia and connect muscles across joints along 14 different arrangements (Figure 2). Because the epimysium, perimysium, and endomysium are connected to each other, muscle spindles attached to the endomysium are over activated, resulting in increased alpha-motor neuron excitability. Moreover, poor gliding of muscle fiber results in reduced muscular flexibility and output.
Table 1. Causes of fascial degeneration.
|
Mechanical |
Acute: sprain, fractures, direct trauma Chronic: excessive use, posture, work, sports |
|
Physical |
Temperature: heat, cold, wind, humidity Mental strain: anguish, conflict, depression |
|
Chemical |
Nutrition: overnutrition, unbalance, addiction Endocrine: hormones |
|
Infection |
Metabolism |
|
Immobilization: |
Development of abnormal small networks between collagen fibers Alteration of collagen turnover mechanics (synthesis and degradation) Cleavage of new collagen fibers Change in quantity and quality of amorphous substance due to reduced water and glycosaminoglycans (GAGs) |
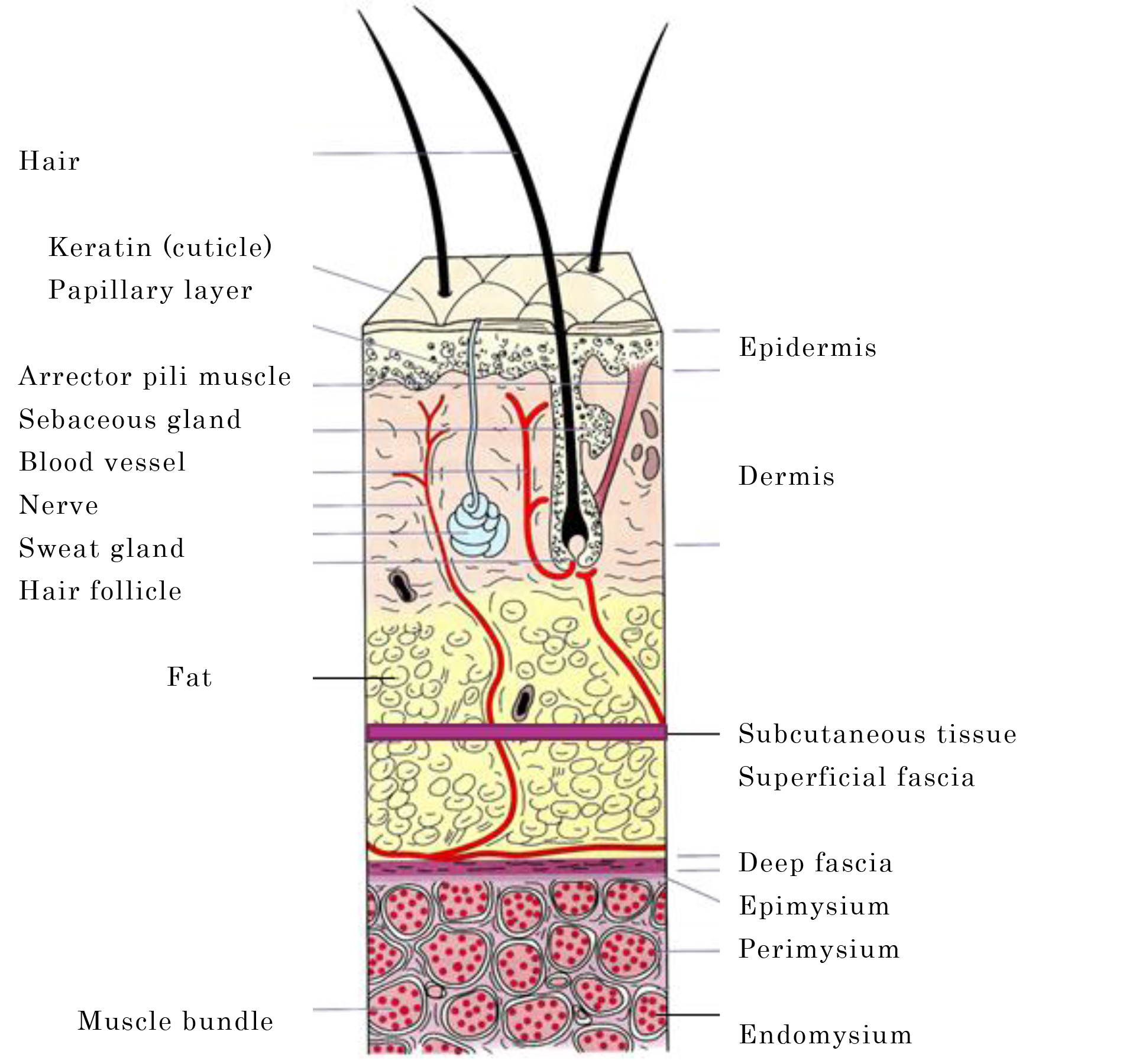
Figure 1. Superficial fascia, deep fascia, epimysium, perimysium, endomysium
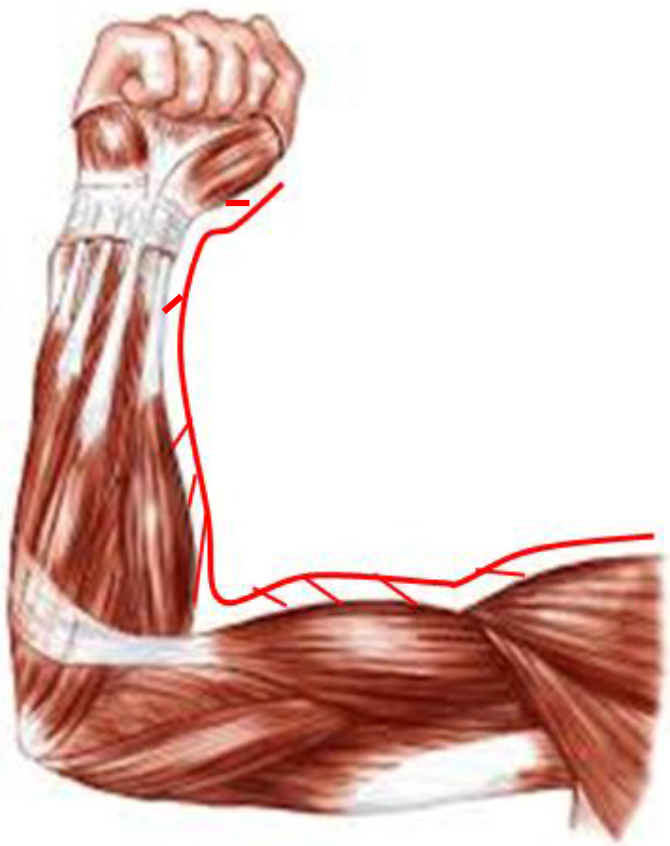
Figure 2. Muscle fibers enter from epimysium into the deep fascia
All traction forces exerted by muscle spindles on the endomysium converge simultaneously on the epimysium. In the simplest fascial unit, traction forces are transmitted along the same muscle and converge on the midpoint. Even in a more complex fascial unit formed by many different muscle motor units, these forces converge on a single point. This exact point on the epimysium where muscle force vectors converge is referred to as the Center of Coordination (CC). The point where vectors from two adjacent fascial units converge in a multiplanar, diagonal, composite motion method (anterior-lateral, anterior-medial, and rear-lateral, rear-medial) is referred to as the Center of Fusion (CF). The human body can be divided into 14 segments: scapula (sc), humerus (hu), elbow (cu), carpus (ca), and fingers (di), which constitute the upper limbs; head (cp), neck (cl), thorax (th), lumbar (lu), and pelvis (pv), which constitute the trunk; and hip (cx), knee (ge), talus (ta), and toes (pe), which constitute the lower limbs. Abbreviations for body segments are written in Latin [1,2] (Table 2).
Table 2. Body segments and terms used to represent their abbreviations.
|
Japanese |
Latin |
Latin |
English |
Anatomical parts included |
|
手指 |
DI |
Digiti |
fingers |
Intercarpal and interphalangeal joints, interosseous muscles of the hand |
|
手根 |
CA |
Carpus |
wrist |
Radiocarpal joint, extensor carpi radialis muscle, and extensor carpi ulnaris muscle |
|
肘 |
CU |
Cubitus |
elbow |
Elbow joint, brachial fascia, biceps brachii muscle, triceps brachii muscle, brachioradial muscle |
|
上腕 |
HU |
Humerus |
shoulder |
Glenohumeral joint, deltoid muscle, biceps brachii muscle, supraspinous muscle |
|
肩甲骨 |
SC |
Scapula |
scapula |
Scapulothoracic and collar joints, trapezius muscle, serratus anterior muscle, rhomboideus muscle |
|
頭部 |
CP |
Caput |
head |
Skull and temporomandibular joint, eye muscles, temporalis muscle |
|
Neck |
CL |
Collum |
neck |
Cervical spine, cervical fascia, iliocostalis cervicis muscle |
|
胸郭 |
TH |
Thorax |
thorax |
Thoracic spine, thoracolumbar joint, iliocostalis thoracis muscle, pectoral muscles |
|
腰部 |
LU |
Lumbi |
lumbar |
Lumbar spine, fascia, iliocostalis lumborum muscle, rectus abdominis muscle |
|
骨盤 |
PV |
Pelvi |
pelvis |
Sacroiliac joint, pubic symphysis, gluteal muscles, abdominal oblique muscle, rectus abdominis muscle |
|
股 |
CX |
Coxa |
thigh |
Hip joint, thigh, internal obturator muscle, pubic muscle, piriform muscle |
|
膝 |
GE |
Genu |
knee |
Knee joint, femoral fascia, quadriceps femoris muscle, biceps femoris muscle |
|
距骨 |
TA |
Talus |
ankle |
Ankle joint (talocrural joint), lower leg fascia, gastrocnemius muscle, tibialis muscle |
|
足趾 |
PE |
Pes |
foot |
Intertiparal and interphalangeal joints, fascia, interosseous muscles of foot |
There are 6 arrangements of CCs and 8 arrangements of CFs connecting these segments; thus, at least one of these 14 arrangements is affected in fascial dysfunction. The wavy collagen fibers of the epimysium and perimysium/endomysium connect to the tendon. When the tendon stimulates mechanoreceptors and nociceptors in a joint, the patient feels pain around the joint. The area where the patient feels or perceives pain is referred to as the Center of Perception (CP). Thus, therapists should be aware that the problem is not in the joint, but in the fascia. Successful treatment of fascial dysfunction relieves muscle/fascial pain and improves muscular output/flexibility and motor paralysis, resulting in improved exercise performance and activities of daily living.
Treatment of Fascial Dysfunction
Treatment for fascial dysfunction includes muscle pain relief as an indirect approach, and myofascial release and Fascial Manipulation® (FM) as direct approaches (Table 3). General assessments include current history of pain and concomitant pain, detailed history taking, alignment, Range of Motion (ROM) during exercise, muscle strength, abnormal sensation, and determination of the site of pain by palpation. Motion assessment (active/passive motion, stretching, resistance exercise) is then performed to determine whether there is any pain, ROM restriction, and/or muscle weakness. These assessments are combined with assessment of CCs and CFs by palpation to assess each segment and arrangement. Balance between agonist and antagonist muscles should also be considered when performing treatment.
Table 3. Therapeutic techniques for fascial dysfunction.
|
Procedure |
Description |
|
Muscle pain relief (MPR)
|
A myofascial treatment technique based on strain-counterstrain with some original modifications developed by Takei taking into account the fascial arrangement. This technique is effective for relieving pain in center of coordination (CC) on epimysium where vectors of muscle strength converge, by having a patient passively take an easy posture that is least painful and thereby causing the muscle spindle to be shortened passively to reduce or suppress inappropriate proprioceptive activity. |
|
Myofascial release
|
This technique is intended to influence the fascial tissue all over the body and aims to release and unravel twisted fascia, change the viscosity of the fascial matrix, and adjust muscular/fascial balance, rather than simply stretching the fascia. Concepts of CC and fascial arrangement have further improved its therapeutic effect. |
|
Fascial manipulation® fascial manipulation® |
Therapeutic targets are the CC and the center of fusion (CF), which is a wider region or a point where forces from multiple fascial units converge. For a densified CC, assessment and treatment should be performed along the fascial arrangement. Take sufficient time to rub each CC to correct the viscosity of matrix. Balance between agonist and antagonist muscles should also be taken into consideration. CFs are involved in the coordination of complex movements. Assessment and treatment should be performed along the diagonal and spiral fascial lines. Apply lower pressure than for CCs to increase friction glide. |
Muscle Pain Relief
Muscle Pain Relief (MPR) is a technique based on the therapeutic principle of Strain-Counterstrain (S-CS) with some original modifications. The technique was developed by Takei as a treatment for muscle/fascial pain, taking into account the fascial arrangement. S-CS, also referred to as ‘positional release,’ is a technique used to relieve pain by moving a body part affected by somatic dysfunction to an easy, less painful position to reduce or suppress the inappropriate proprioceptive activity responsible for the somatic dysfunction [4–12]. However, this technique does not involve whole-segment assessment/treatment along the anatomical fascial arrangement and focuses on treating muscle pain at each part. Moreover, in S-CS, “tender points” are considered to indicate somatic dysfunction, whereas the therapeutic targets of MPR are CCs on the epimysium where muscle force vectors converge. CCs are scientifically defined points based on the anatomical fascial arrangement [1,2].
Therapeutic Principle
A muscle spindle is located in parallel with the course of muscle fibers and senses the length of a muscle and the degree of change thereof [13,14]. In the middle and adjacent parts of the muscle spindle are sensory receptors known as the primary and secondary endings, which are innervated by group Ia and II sensory nerve fibers, respectively. The middle part of the muscle spindle is non-contractile and contains a receptor formed by annulo-spiral endings while both its ends form a contractile intrafusal muscle fiber that connects to an extrafusal muscle fiber. The intrafusal muscle fiber at both ends is innervated by gamma-motor neurons, which only innervate intrafusal muscle fibers, and beta-motor neurons that innervate both the extra- and intrafusal muscle fibers via a single axonal branch. Activation of these neurons causes both ends of the spindle to contract. This force is too weak to cause muscle tension but does increase the tension of the muscle spindle, thereby enhancing its sensitivity as a receptor. Excitation of the muscle spindle or gamma efferent fibers and subsequent muscle contraction results in increased impulse from the primary endings (group Ia fibers). Taking a joint position that allows this strained and activated muscle spindle to be shortened passively leads to decreased afferent firing from the primary endings and decreased alpha- and gamma-motor neuron firing in the central nervous system, resulting in relaxation of the extrafusal muscle fibers [4–8, 15–17].
General principles of treatment
Therapists with minimal experience should try various postures and identify those which are comfortable and uncomfortable based on feedback from the patient. The optimal posture should relieve pain. If pain/tenderness is successfully relieved, the patient will perceive it distinctly. As more experience is gained, it will be easier to feel changes with the fingertips and find an ideal posture. Therapists with more experience can tell that the ideal posture has been achieved even when the patient is still in pain. Even such patients are likely to have pain relief in about 30 seconds.
Actual treatment procedure
The MPR techniques are applied to CCs all over the body. In MPR, tender points in specific areas of the musculoskeletal system are identified and used for both diagnostic and therapeutic monitoring purposes. Once a CC is identified, it is necessary to find a position that can reduce both tenderness and the sensitivity of the tissue felt by the therapist. What is important here is to understand the action of each muscle three-dimensionally. It is important to find a position that can reduce pain three-dimensionally, taking into account composite factors such as flexion/extension, adduction/abduction, and external/internal rotation, rather than a position that simply shortens the muscle to the maximum extent. During treatment, keep the finger on the CC, but with a lighter touch than during diagnosis, to feel changes in the tissue. Feel with the fingertips that tension is released and ask the patient if pain/tenderness is released while pressing the point intermittently. Hold this posture for about 90–120 seconds. Then, slowly return the patient to the normal posture and perform reassessment. The following part of the section describes example treatment procedures for Antemotion (AN) of the upper limbs.
Example treatment cases
AN-SC: Pectoralis minor (Figure 3)

Figure 3. MPR for AN-SC (pectoralis minor)
CC: Located inferior to the coracoid process and on the belly of the pectoralis minor and the coracoclavipectoral fascia.
CP: Pain in the shoulder, clavipectoral fascia, and acromioclavicular joint (CC and CP are close).
Treatment position: Supine position. The CC-side upper limb is placed across the front of the body. Scapula: Tilted anteriorly, rotated inferiorly, and depressed.
AN-CU: Biceps brachii (Figure 4)

Figure 4. MPR for AN-CU (biceps brachii)
CC: Located just below the deltoid attachment and lateral to the belly of the biceps brachii.
CP: Pain at the anterior elbow, often at the epicondyle or distal biceps brachii tendon.
Treatment position: Supine position. Shoulder joint: Flexed to 90°, slightly to moderately abducted (or slightly to moderately adducted for the short head). Elbow: Moderately flexed. Forearm: Supinated.
Myofascial Release (MFR)
The purpose of MFR is to restore the normal function of muscles and other structures by reversing fascial twisting and to improve the mobility and stretchability between muscles or between muscles and other structures. The deepest fascial tissue forms a dural tube that wraps and supports the central nervous system and impaired dural mobility may limit the physiological movement of the skull and sacrum, causing various forms of dysfunction [18–21]. Because the fascial tissue forms a systemic network, MFR is often combined with cranio-sacral therapy [18]. Although similar therapeutic techniques have traditionally been applied in osteopathy, the MFR technique described here was systematically established by John F. Barnes et al. and is intended to release and unravel fascial twisting, rather than simply stretching the fascia [18,22–25]. Based on this technique, Takei et al. incorporated the concepts of CCs and fascial arrangement to establish their original therapeutic principles and techniques (Takei’s concept). This modification has made MFR a more effective technique.
What is “release”?
The objective of MFR, in particular, deep myofascial release, is to release densified and cross-linked collagen and elastin fibers and change the viscosity of the fascial matrix (intercellular material) from gel to sol. Barriers formed by the collagenous component cannot be corrected forcibly. Instead, applying gentle and sustained stretching and pressure can change the viscosity or density of the matrix and release the restriction caused by collagen fibers, resulting in a change in tissue length. First, apply pressure down to the deep fascia. Then, while keeping the pressure, apply gentle stretching motions to the site of fascial restriction, causing the elastic component to be stretched by the initial stretch applied to the fiber complex. The elastic element is slowly pulled like an elastic or spring coil until the hand applying the stretch stops at a tough barrier formed by the collagenous component. It should be kept in mind that elastin fibers have shape-memory properties and if stretching stops here, they return to their original length due to elasticity. Although barriers formed by the collagenous component cannot be corrected forcibly, applying sustained stretch can cause gradual stretching of collagen fibers due to the viscoelasticity of elastin fibers [26]. The stretched elastin fibers allow the tissue to regain its original shape and flexibility, resulting in restoration of the proper biomechanical alignment of the skeleton. Barriers formed by the collagenous fibers cannot be corrected forcibly. Lower load (gentle pressure) is more effective than higher load (fast, pressure applied) in changing the viscosity of the matrix [18]. Applying gentle and sustained stretching and pressure over 90 seconds to 3 minutes (5 minutes maximum) can change the viscosity or density of the matrix and release the restriction caused by collagen fibers, resulting in a change in the tissue length.
Precautions during release
After successful myofascial release, many patients experience an emotional change known as “somatoemotional release.” Just as emotional stress causes physical tension, physical stress causes emotional tension. Thus, releasing the fascial tissue from physical stress also results in emotional release [18,19,21].
Goal of myofascial release
The goal of myofascial release is to release fascial restriction and restore the overall musculoskeletal balance leading to a balanced posture. Acquisition of a structurally balanced posture will permit normalization of the center-of-gravity line and the symmetrical functioning of the entire musculoskeletal system. Applying gentle stretching to the fascial restriction elicits heat, which is a vasomotor response that increases blood flow in the affected area, improves lymph drainage, reorganizes the fascial tissue, and most importantly resets the sensory mechanism of soft-tissue proprioception [18,19–21]. This activity will reprogram the central nervous system, allowing a normal functional range of motion without eliciting old pain patterns [27]. The final goal is to achieve optimal function and performance with the least amount of energy. Because this technique is mild, MFR is applicable to various signs and symptoms. Systemic contraindications include malignant tumors/cancer, aneurysms, acute rheumatoid arthritis, and systemic/local infection; local contraindications include hematomas, open wounds, sutured wounds, and fracture sites during the healing process.
Actual treatment procedure
The three basic MFR techniques are 1) longitudinal release, 2) transverse release, and 3) pulling or traction (Fig. 5). Longitudinal release is a technique used to stretch the fascia while gently applying pressure so as to sandwich the CC, taking into account the fascial arrangement, and to keep stretching after feeling the restriction of elastin fibers until the restriction of collagen fibers is released and myofascial release is achieved. Transverse release is a technique used to release the fascia on the transverse plane while simultaneously feeling the ventral and dorsal connections of the deep fascia. Pulling is a technique that is used to easily move the upper or lower limbs in various directions while releasing the fascia distally. While performing release, the therapist should be relaxed and feel as if their palm or finger pulps were fused with the patient’s skin. While applying pressure down to the deep fascia while stretching the skin, the deep fascia is also stretched. In the initial phase of release, the elastic component is slowly pulled like a spring coil. Then, maintain the pressure for 90 seconds to 3 minutes (5 minutes maximum) to release the collagen component, causing the tissue to soften like melting butter. Pressure reaches the deeper layers gradually. The time required to complete the procedure will decrease with improved technique. Successful release will allow elastin, a constituent of elastin fiber, to help restore the original shape and flexibility of the tissue. The following part of this section describes representative treatment procedures for Lateromotion (LA) of the upper limbs.
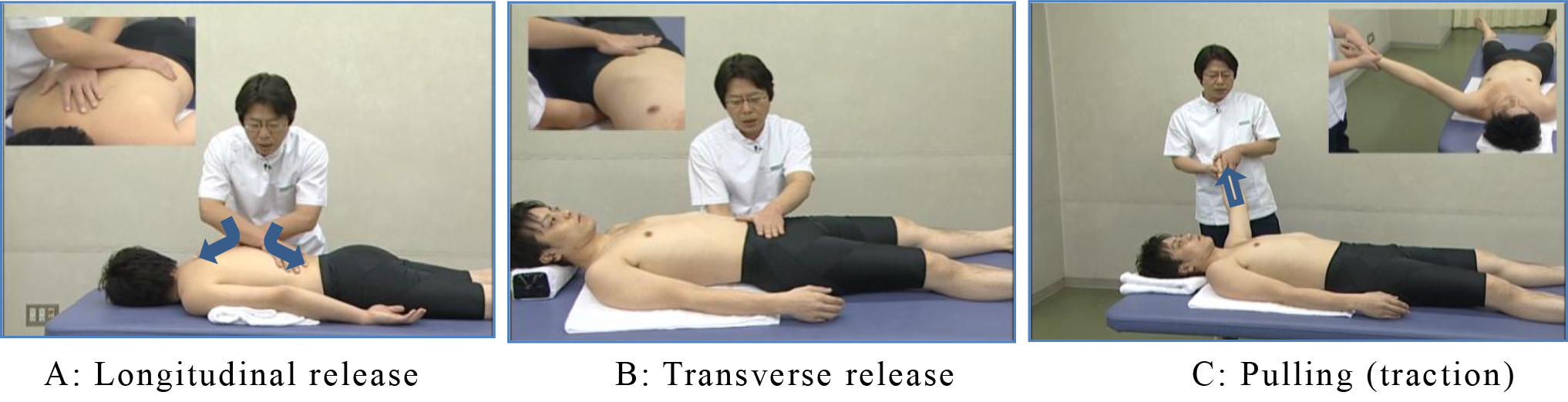
Figure 5. Three basic techniques for myofascial release
Representative treatment cases
LA-CX: Tensor Fascia Lata (Figure 6)

Figure 6. Release of LA-CX (tensor fascia lata)
CC: Located inferior to the anterior superior iliac spine and on the tensor fascia lata.
CP: Pain in the lateral thigh around the tensor fascia lata. Numbness at a lower part of the lateral thigh.
Treatment position: Lateral position, with the lower leg placed forward and the upper leg placed slightly backward. Place your hands crossed over the CC (cross-hand technique) to apply pressure and stretch.
LA-TA: Extensor Digitorum Longus (EDL) (Figure 7)
CC: Located between the proximal one-third and middle one-third of the lower leg, anterior to the fibula and on the EDL. Another located on the peroneus tertius.
CP: Pain in the lateral ankle. Pain secondary to ankle sprain.
Treatment position: Lateral position. Apply pressure and stretch to the EDL at the middle one-third of the lower leg (slightly above the mid-point) and anterior to the fibula.

Figure 7. Release of LA-TA (extensor digitorum longus)
Fascial Manipulation®
The therapeutic principle of FM consists of mechanical (movement – friction), physical (heat – inflammation) and chemical (metabolism – repair) elements. The therapeutic targets are CCs and CFs. CCs are located in the 6 fascial units that move various body segments in 3 spatial planes (anterior and rearward movements in sagittal plane, medial and lateral movements in frontal plane, and internal and external rotation in horizontal plane). CFs are involved in multiplanar composite movements on diagonal lines and spirals (anterior-lateral [AN-LA], anterior-medial [AN-ME], rear-lateral [RE-LA], and rear-medial [RE-ME]). Differences between CC and CF are shown in
table 4. FM is also effective in evaluating and treating the musculoskeletal system affecting internal dysfunction, including visceral, vascular, and glandular dysfunction; in treating sensory organs in the head, including the face; and in treating the superficial fascia for lymphatic/immunological, dermatological/thermoregulatory, fat/metabolism, and neurogenic/psychogenic disorders [28]. An alternative treatment approach for lymphatic/immunological, dermatological/thermoregulatory, fat/metabolism and neurogenic/psychogenic disorders is to divide each of the trunk, upper, and lower limbs into 4 areas (AN-LA, AN-ME, RE-LA, and RE-ME) and treat the superficial fascia in each area.
Table 4. Differences between center of coordination (CC) and center of fusion (CF)
|
CC |
CF |
|
Located on the muscle belly and coordinates fascial units through the epimysium, perimysium, and endomysium. |
Located on the tendon and coordinates the motion method through the retinaculum and fascial spiral. |
|
Located in body parts that correspond to the three spatial planes. |
Located in the intermediate zone (diagonal line) between two planes near the joint. |
|
Mobilized when force is required or when the muscle insertion into the fascia is tensioned (arranged). |
Mobilized by retinacular tension applied either directly (via the tendon) or indirectly (via movement of the bone to which the retinaculum is attached). |
Actual assessment procedure
Fascial dysfunction may occur on the fascial arrangements where fascial units in each segment involved in local pain are arranged on the frontal, sagittal, and horizontal planes (Figure 8); the fascial diagonal lines on these planes (Figure 9); and the fascial spirals involved in extensive pain (Figure 10). Motion assessment is performed to assess the entire bone-nerve-myofascial complex or individual fascial units instead of individual muscles, by moving each segment in a specific direction. Each CC is located slightly away from their corresponding CPs and pain is only detectable on assessment by palpation. Based on the results of motion and assessment by palpation, it is necessary to identify densified and degenerated fasciae, treat the fasciae to reverse fascial degeneration, and continue verifying hypotheses and results.
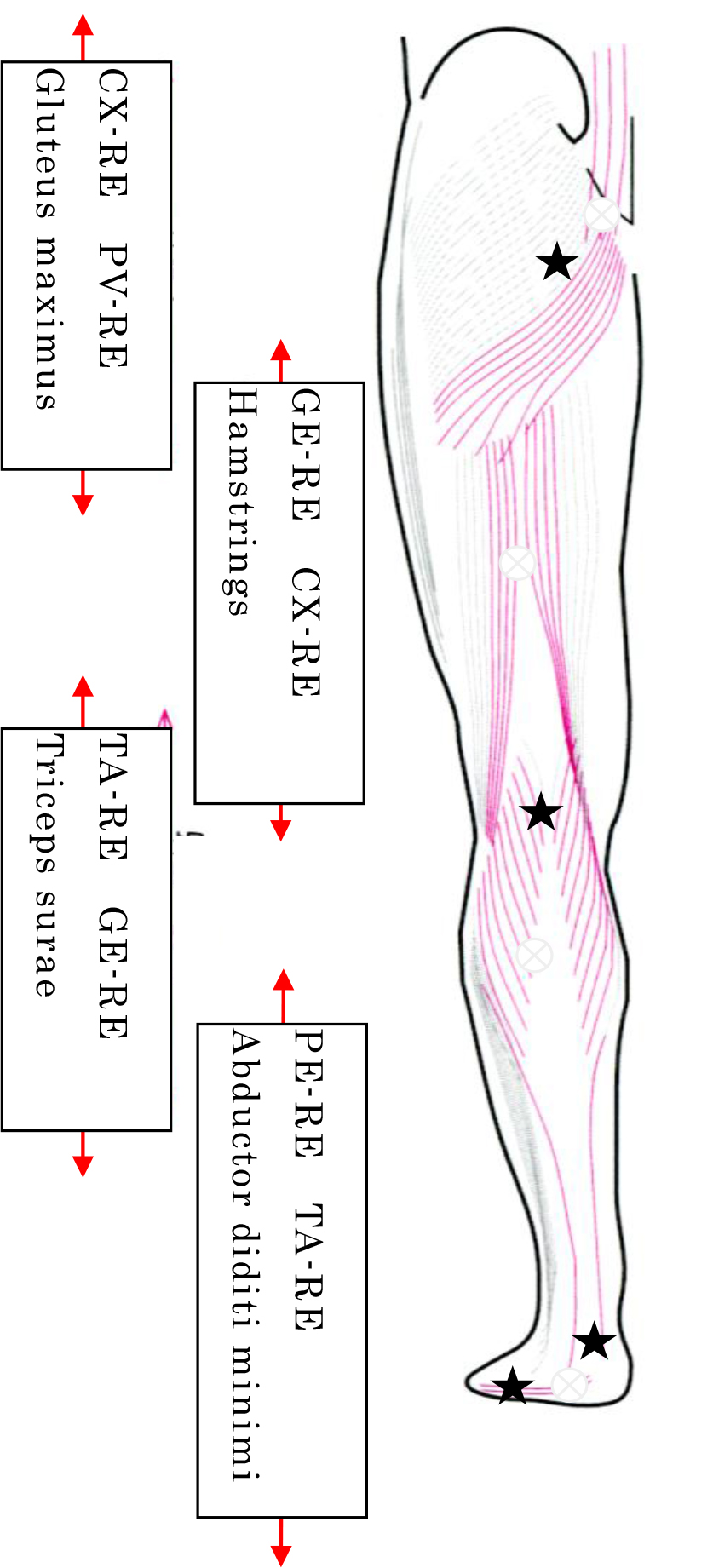
Figure 8. Example fascial arrangement: Sagittal view of the fascial arrangement involved in backward movement of the lower limb (adapted from reference 1 with some modifications)
Center of coordination: ![]() Center of perception (site of pain):
Center of perception (site of pain): ![]()
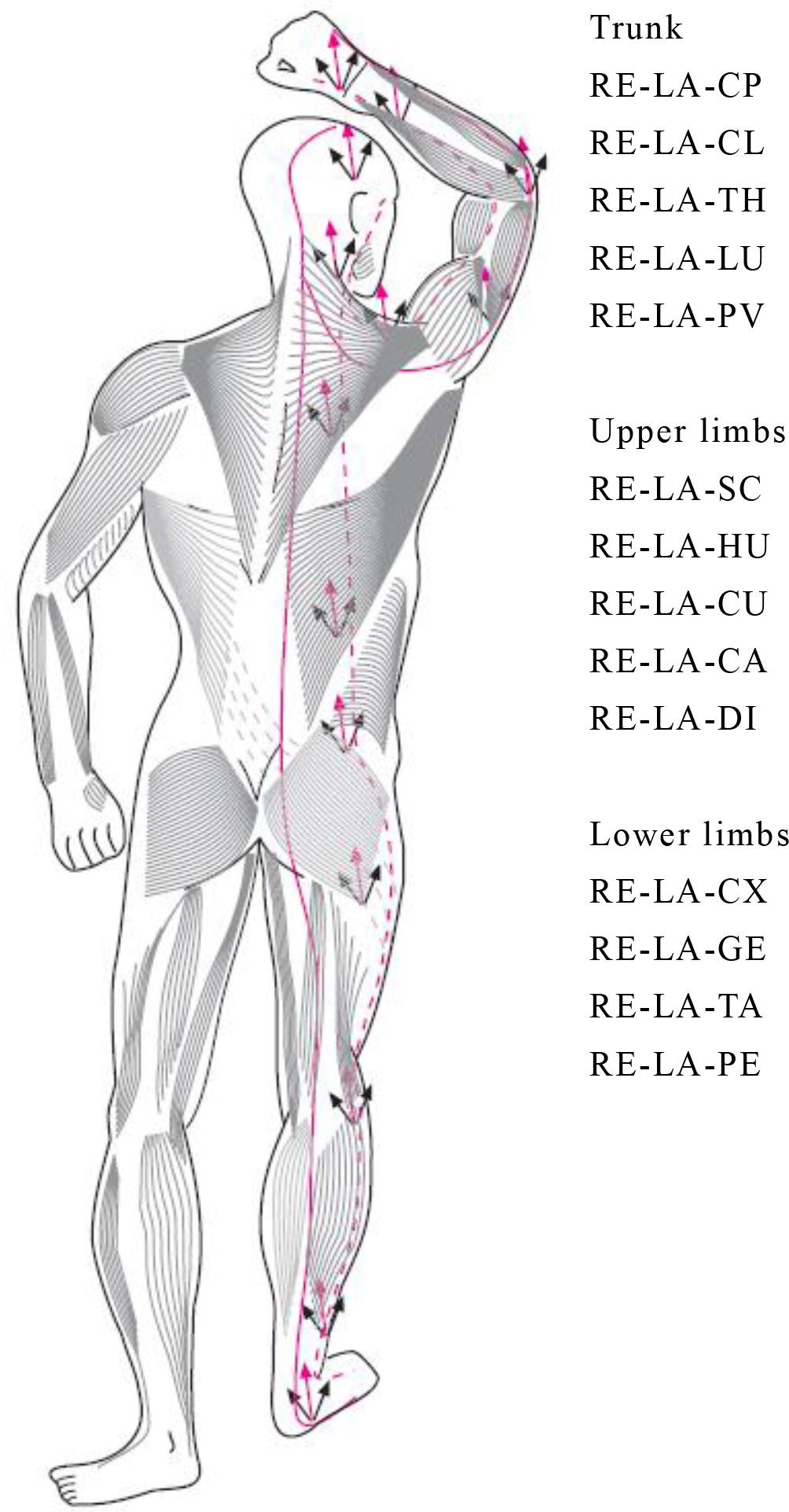
Figure 9. Example diagonal lines: Centers of fusion (CFs) on rear-lateral diagonal lines2)
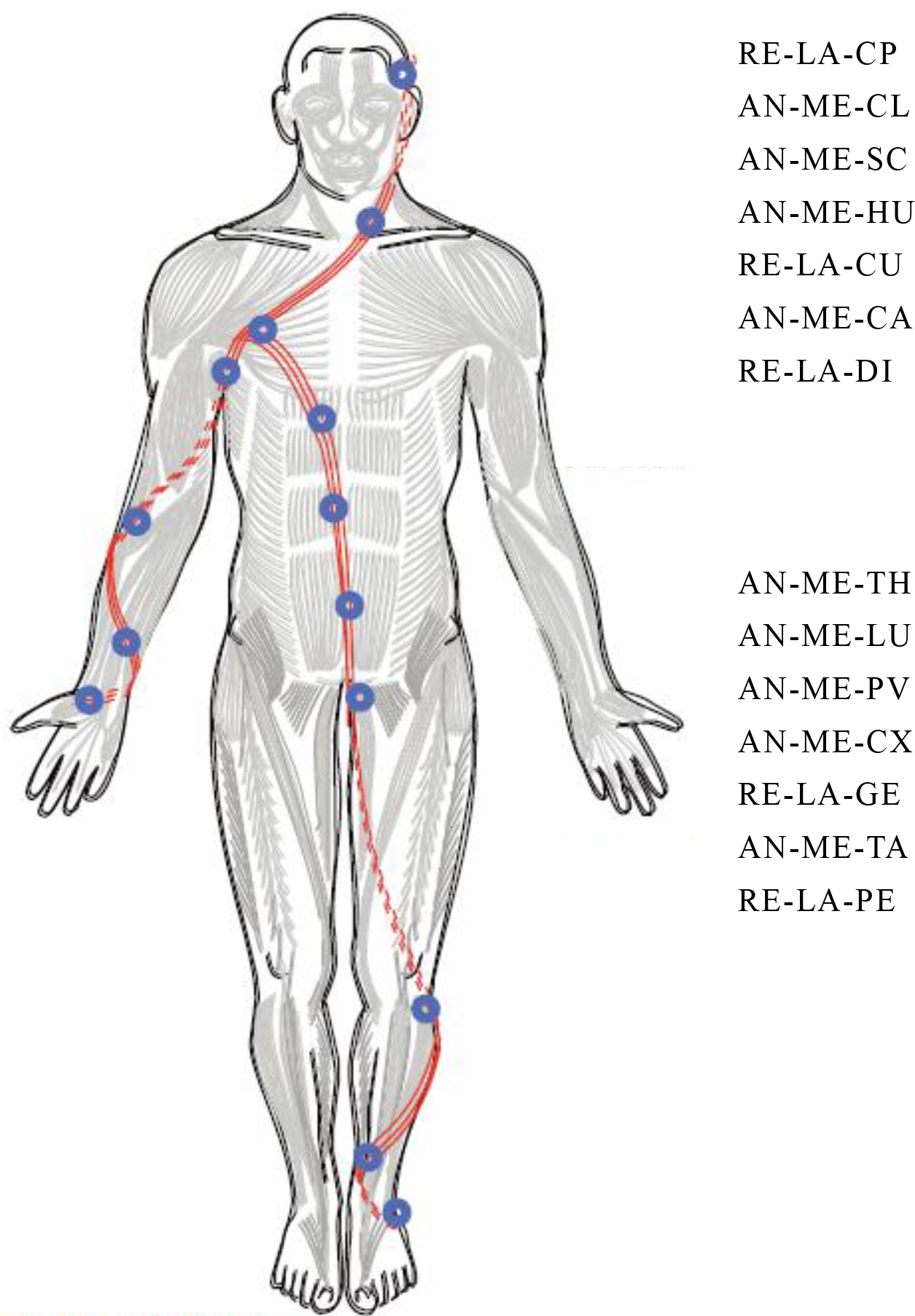
Figure 10. Example fascial spiral: A RE-LA (rear-lateral) spiral originating from the rear lateral aspect of the hand and foot.
Actual treatment procedure
FM should be performed on a densified area that needs to be treated by applying deep pressure to the area (CC or CF) while applying friction for a sufficient length of time to generate heat. This heat helps correct the viscosity of the matrix and initiates inflammatory processes required for healing. This technique should be continued until fascial correction is achieved and pain resolves. Increased temperature promotes the gel-to-sol transition and results in a corrected fascial matrix. In general, the viscosity transition of a densified fascia can be achieved in several minutes. Sudden release of free nerve endings results in reduced densified loci, leading to improved motor coordination, normalized joint motion trajectory, and subsequent reduction of associated pain. This results in elimination of a fibronectin network that interferes with the functionality of CCs. Immediately after treatment, patients may perceive improvement in symptoms and local warmth around the treated area. With no swelling, they feel even better than before treatment. A small depression due to change in loose connective tissue may occur in this area. After 10 minutes, some patients may notice worsening of symptoms and local pain. This is due to increased blood flow to the area and swelling formed as a consequence of the exudation phase. FM prevents matrix binding to allow for a new orientation of fibroblasts. During several hours after the fascial inflammation phase, neutrophils appear following macrophages and are removed simultaneously with newly formed necrotic material. Myofibroblasts are activated and produce new type-III collagen fibers.
During the following 3 days, a small hematoma may appear at the treated area, which may worsen symptoms temporarily depending on predisposing factors. At this time, the use of anti-inflammatory compresses or medications should be avoided because they inhibit normal inflammatory reaction. Patients in good condition should also refrain from walking longer than usual or going shopping or to a fitness gym. By 5 days after treatment, reduced local pain, improved fascial tension balance, and resolution of symptoms and swelling should be observed. During the next 20 days, the initial type-III collagen fibers are gradually arranged along the traction line and are replaced by more stable type-I collagen fibers. It is important to inform patients in advance of the possibility of these reactions.
Example treatment cases
AN-GE: Lateral aspect of rectus femoris (Figure 11)

Figure 11. Fascial manipulation on AN-GE (lateral aspect of rectus femoris)
CC: Located at half of the length of the thigh and on the vastus intermedius between the rectus femoris and vastus lateralis.
CP: Pain in the inguinal region and the medial thigh. Pain in the muscles attached to the pubic bone.
Treatment position: Supine. Apply pressure and friction with a knuckle or elbow placed on the fascia lata in the lateral aspect of the rectus femoris between the patella and the inguinal ligament.
RE-PV: Iliocostalis lumborum (Figure 12)

Figure 12. Fascial manipulation on RE-PV (iliocostalis lumborum)
CC: Located at the L5 level and medial to the posterior superior iliac spine on the quadratus lumborum muscle originating from the iliolumbar ligament.
CP: Pain at a site medial to the sacrum, piercing in nature, may diffuse along the posterior thigh/lower leg.
Treatment position: Prone. Apply pressure and friction with the elbow placed between the fifth lumbar spine and the anterior superior iliac spine.
RE-LA-LU: Latissimus dorsi (Figure 13)

Figure 13. Fascial mobilization on RE-LA-LU (latissimus dorsi)
CF: Located at the center of the latissimus dorsi at the costal attachment of the upper margin of the serratus posterior inferior and the iliocostalis.
CP: Back pain occurs on torsion, lateral bending, or extension.
Treatment position: Prone. Apply a lower pressure and a slightly broader friction than for CC treatment (fascial mobilization) to the center of the latissimus dorsi at the costal attachment of the upper margin of the serratus posterior inferior and the iliocostalis.
Three treatment techniques for fascial dysfunction were described. Of these, muscle pain relief is an indirect treatment technique and is less effective than others for physical improvement of fascial dysfunction. Still, causing no inflammatory reaction, this technique is effective for persons with low pain threshold, children, the elderly, and athletes scheduled to participate in an event on the same or following day. Myofascial release and FM are both direct treatment techniques, although the former is more effective for those people sensitive to pain and those athletes scheduled to participate in an event on the following day. FM is most likely to cause inflammatory reaction among these techniques, and therefore requires sufficient patient orientation and accurate assessment. Therapists should also be able to select the most suitable technique for each patient.
References
- Takei H (2011) Fascial Manipulation, Theoretical. Ishiyaku Publishers Tokyo.
- Takei H (2011) Fascial Manipulation, Practical. Ishiyaku Publishers Tokyo.
- Takei H (2013) Fascial manipulation. In: Shimada T, Arima Y and Saito H (eds.) Physiotherapy practice based on clinical thinking: Guidance for Clinical Application of Recent Findings for Unexperienced and Young Physical Therapists – Musculoskeletal physiotherapy, Bunkodo, Tokyo, 46–60.
- Jones LH, Kusunose RS (1995) Strain and Counterstrain. Course taken in San Francisco, Jones Institute, INC.
- Kusunose RS (2003) Strain and Counterstrain. Advanced and cranials syllabus. Course taken in Seattle, Jones Institute, INC.
- Jones LH (1995) Jones Strain and Counterstrain. Jones Strain-CounterStrain, Inc., Boise, ID.
- Jones LH: Strain and counterstrain. The American Academy of Osteopathy, Indianapolis, IN, 1981.
- Kusunose RS (1993) Strain and counter strain. In: Basmajian JV, Nyberg R (eds.), Rational manual therapies. Williams & Wilkins,Baltimore 323–333.
- Jones LH (1964) Spontaneous release by positioning. DO 1:109–116.
- Jones LH (1973) Foot treatment without hand trauma. Journal of the American Osteopathic Association 72: 481–489.
- Mitchell FL, Moran PS, Pruzzo NA (1979) An evaluation and treatment mannual of osteopathic muscle energy procedures. Mitchell, Moran and Pruzzo,Valley Park, Pg-no: 1–3.
- Korr IM (1975) Proprioceptors and Somatic Dysfunction. Journal of the American Osteopathic Association 74: 638–650.
- Takei H (2004) Structure of Locomotor System. Kinematics (Edited by Maruyama H). Chugai-Igakusha, Tokyo, Pg-no: 5–54
- Takei H (2008) Color Atlas of Palpation and Functional Anatomy. Vol.2. Bunkodo, Tokyo.
- Lee DG Principles and practice of muscle energy and functional techniques. In: boyling JD & Palastanga N (eds.), Grieve’s modern manual therapy(2nd ed), Churchill.
- Sydenham RW (1994) Manual therapy techniques for the thoracolumbar spine. In: Donatelli RA, Wooden MJ (eds.), Orthopaedic Physical therapy(2nd ed), Churchill Livingstone, New York, Pg no: 421–465.
- Nakamura Y (1996) Reflexes. Edited by Hoshi T et al., Review of Medical Physiology, Maruzen Publishing, Tokyo, Pg no: 123–132.
- Barnes JF (1990) Myofascial release. John F.barnes,P.T. and Rehabilitation Services, Inc., Pennsylvania.
- Swenson C (1995) Craniosacral therapy. Course taken in Mineapollis,The upledger institute, INC.
- Upledger JE, Vredevoogd JD (1983) Craniosacral therapy. Eastland Press Seattle.
- Upledger JE (1987) Craniosacral therapy. Eastland Press Seattle.
- Takei H (2007) Myofascial Release In: Development of Therapeutic Techniques of Different Categories, 2nd Edition, Edited by Nara I et al., Kyodo Isho Shuppan, Toyo, Pg no: 95–128.
- Takei H (2005) Myofascial Release. In: Advanced Illustrated Physiotherapy Technical Guide, Edited by Hosoda K et al., Bunkodo, Tokyo, Pg no: 709–729.
- Takei H (2000) Overview of myofascial release approaches. Manipulation 15: 14–20.
- Ward RC (1993) Myofascial release concepts. In: by Basmajian JV & Nyberg R (eds.), Rational manual therapies, Williams & Wilkins, Baltimore, Pg no: 223241.
- Twomley L, Taylor J (1982) Flexion,creep,dysfunction and hysteresis in the lumbar vertebral column. Spine 7: 116122.
- Barnes JF, Smith G (1987) The body is a selfcorrecting mechanism.Physical Therapy Forum, 8: 89.
- Takei H (2017) Fascial Manipulation for Internal Dysfunctions (Theoretical). Ishiyaku Publishers, Tokyo.