Abstract
Introduction: Pelvic inflammatory disease (PID) is a syndrome characterized by an infection that usually ascends from the vagina and cervix into the upper genital tract. Chlamydia trachomatis is the predominant causal agent of this type of infection. In Mexico, the prevalence of C. trachomatis infection is still unknown although some reports suggest a frequency of 4 to 10% in the open population, 16% in patients with a history of sexually transmitted diseases and 21% in patients with a PID diagnosis. The objective of the present study was to analyze the epidemiological characteristics of the cases with Pelvic Inflammatory Disease diagnosis attended by the Gynecology and Obstetrics service of the University Hospital “Dr. José Eleuterio González”.
Materials and methods: A descriptive, retrospective and cross-sectional study was carried out; including patients aged 18 to 35 years with a diagnosis of Pelvic Inflammatory Disease attended by the Gynecology and Obstetrics Department of the University Hospital “Dr. José Eleuterio González” from January 1, 2014 to October 1, 2018. The variables evaluated were demographic characteristics, gyneco-obstetric history, risk factors, clinical presentation and the treatment they received.
Results: 221 patients with a diagnosis of Pelvic Inflammatory Disease were included. The average age was 33 ± 7 years. 73 patients (33%) until the time of interrogation had only had one sexual partner, 93 patients (42%) had had 2 to 3 sexual partners and 131 patients (59.28%) mentioned that the IUD was their contraceptive of choice. Regarding the clinical symptoms presented by the patients at the time of the interrogation, 214 patients (96.83%) mentioned presenting pain and 202 patients (91.4%) presented vaginal discharge. 139 patients (63%) received a double antibiotic scheme, 57 patients (26%) received a triple antibiotic scheme. Of the patients who received double treatment scheme, 38 patients (17.19%) were treated with cephalothin and metronidazole. Of the patients who received triple antibiotic scheme, 28 patients (12.67%) were treated with cephalothin; gentamicin and metronidazole. 84 patients underwent a surgical procedure.
Conclusions: With these results, we can conclude the epidemiological characteristics of the patients who are diagnosed with pelvic inflammatory disease. Knowing these characteristics, we can carry out programs to detect risk factors and prevent the incidence and recurrence of PID, in addition to find the treatment scheme that has worked best according to the characteristics of our population.
Keywords
Pelvic Inflammatory Disease; Epidemiology; Treatment; Clinical
Introduction
Pelvic inflammatory disease (PID) is a syndrome characterized by an infection that usually ascends from the vagina and cervix into the upper genital tract. This entity may appear at any time during the woman’s reproductive life, being the adolescence the stage with the highest risk of presentation [1]. It is estimated that 857,000 cases of PID cases are diagnosed annually in the United States, corresponding to an annual incidence rate of 17.2 per thousand women between 15 and 44 years. Over 100,000 women become infertile every year because of this entity and a large proportion of ectopic pregnancies are associated with previous events of PID [2]. Infertility and ectopic pregnancy are caused by tubal damage. The greater the severity and the number of episodes, the greatejr the probability that they appear. Chlamydia trachomatis is the predominant causal agent of this type of infection. Chronic pelvic pain in these patients is secondary to abdominal adhesions [3]. In Mexico, the prevalence of C. trachomatis infection is still unknown although some reports suggest a frequency of 4 to 10% in the open population, 16% in patients with a history of sexually transmitted diseases and 21% in patients with a PID diagnosis using laboratory tests such as cell culture, direct immunofluorescence and molecular techniques [4–7]. The objective of the present study was to analyze the epidemiological characteristics of the cases with Pelvic Inflammatory Disease diagnosis attended by the Gynecology and Obstetrics service of the University Hospital “Dr. José Eleuterio González”.
Materials and Methods
Study Design and Ethical Aspects
A descriptive, retrospective and cross-sectional study was carried out. The Ethics and Research Committee of the Faculty of Medicine and University Hospital of the U.A.N.L. granted previous authorization.
Study population
The information will be recorded in an Excel program database, the variables that will be evaluated are: demographic characteristics: age, educational level and marital status. Gyneco-obstetric history: gravity, parity, age of first sexual intercourse, contraceptive methods, sexually transmitted diseases. Risk factors such as sexually transmitted diseases, previous episodes of IPD, relation to menstruation and clinical presentation such as pain in hypogastrium, abnormal vaginal leucorrhea, fever, nausea and vomiting, pain during intercourse, cervical hemorrhage, pain to the mobilization of the cervix and the treatment they received.
Statistical Analysis
A univariate analysis will be carried out applying the measures of central tendency (mean and median), and measures of dispersion (standard deviation or range), as appropriate for parametric and non-parametric variables, in addition to proportions for qualitative variables. A bivariate analysis will also be done for qualitative variables, as appropriate. An X2 will be made for qualitative variables, and a Student’s T for quantitative variables, with a p <0.05 for statistical significance; in addition, OR and 95% CI will be determined when appropriate. All this supported by pre-designed Excel sheets. For the Software the statistical program EPI-Info 7 is used, which is a free-use program that does not require a license for its management.
Sample size calculation
A sample size calculation was made with a formula for estimating a proportion in an infinite population based on a prevalence of 28% of patients with PID who are evaluated in our setting; for a bilateral confidence of 95% and an accuracy of 10%, we require at least 143 study subjects.
Results
221 patients with a diagnosis of Pelvic Inflammatory Disease were included. The average age was 33 ± 7 years. For the analysis, the data was divided into the risk factors presented by the patients, the clinic presentation at the time of the interrogation and the treatment that was performed: pharmacological or surgical. Among the risk factors, we asked about comorbidities, finding that 160 patients (66%) did not present any comorbidity at the time of interrogation, 28 patients (10.5%) had type 2 Diabetes Mellitus and 12 patients (2.7%) presented Arterial Hypertension in their different stages. In addition, 21 patients (8.60%) presented various comorbidities that because they were presented only in one patient, were not significant with the disease under study (Figure 1).
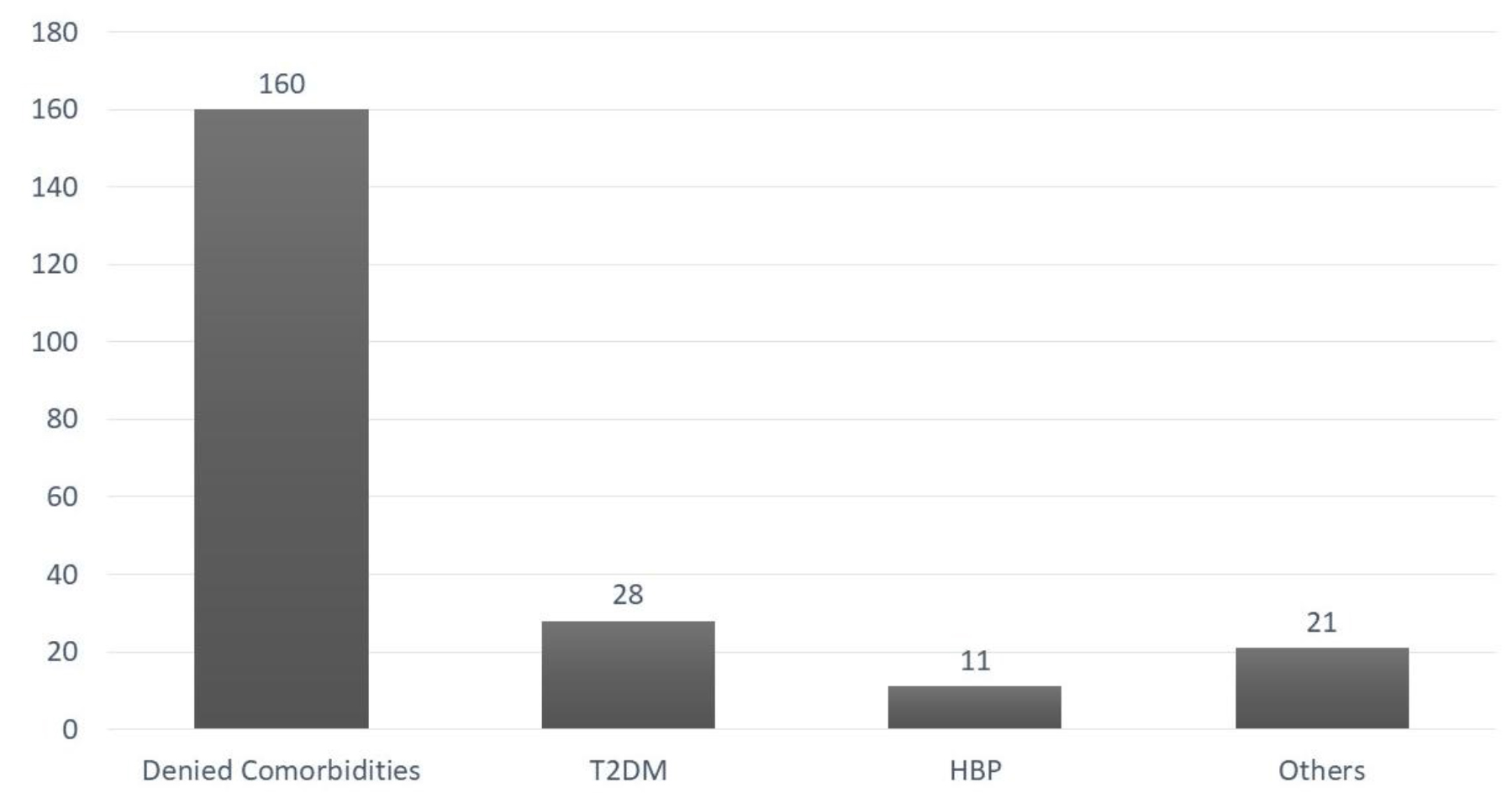
Figure 1. Comorbidities. T2DM, Type 2 Diabetes Mellitus; HBP, High Blood Pressure.
Regarding the non-pathological history such as smoking, it was found that 44 patients (19.91%) were active smokers and 177 patients (80.09%) denied having smoked. For the gyneco-obstetric history, the number of sexual partners was interrogated. 73 patients (33%) until the time of the interrogation had only had one sexual partner, 93 patients (42%) had had 2 to 3 sexual partners, 25 patients (11%) had had 4 to 5 sexual partners, 8 patients (3.62%) had had 5 to 10 sexual partners and 5 patients (11.31%) had had more than 10 sexual partners. (Figure 2) It was asked whether, as a contraceptive method they used an intrauterine device (IUD), 131 patients (59.28%) mentioned that the IUD was their contraceptive of choice and 88 patients (39.82%) mentioned not using the IUD as a contraceptive (Figure 3).
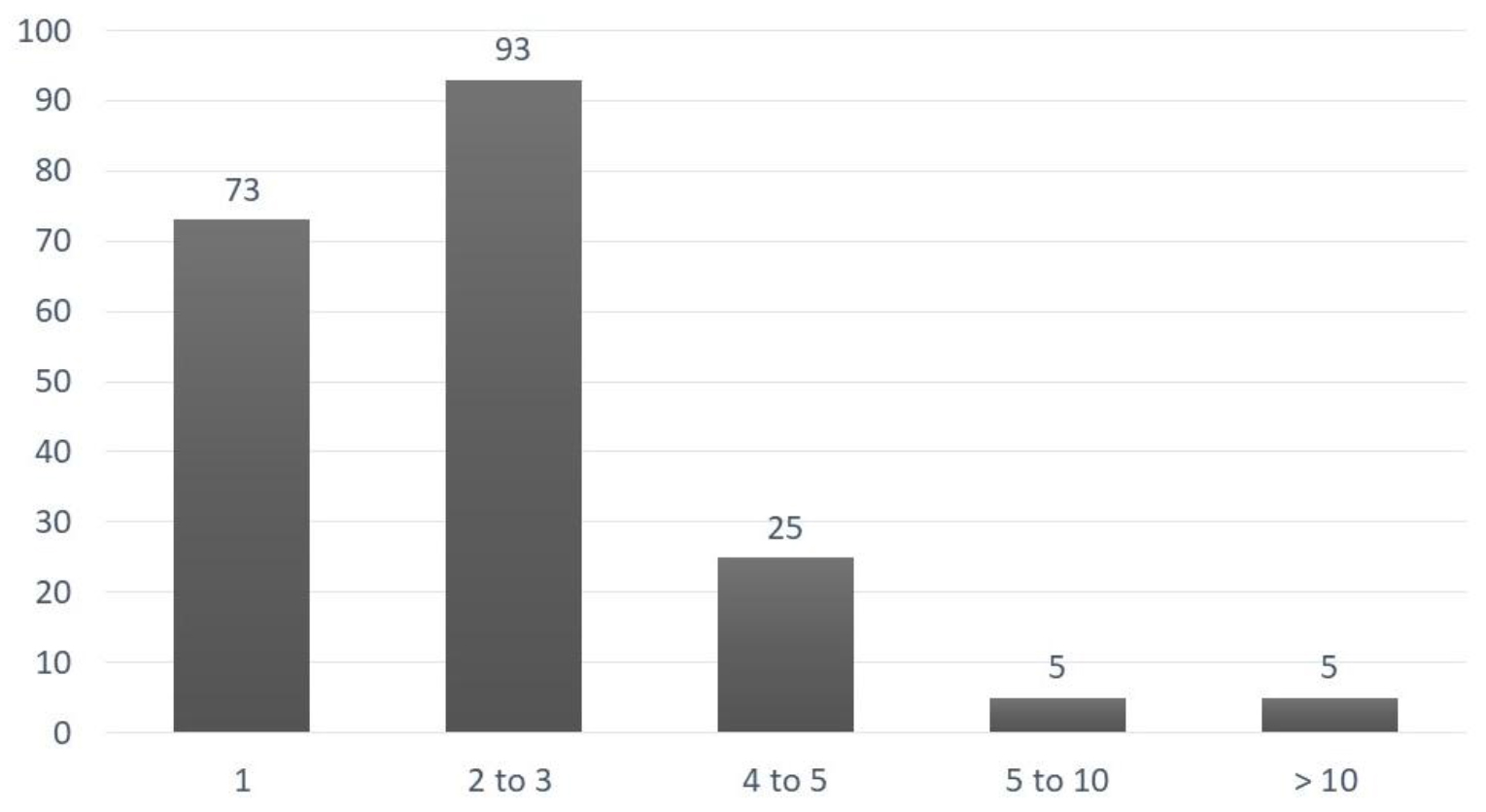
Figure 2. Number of sexual partners
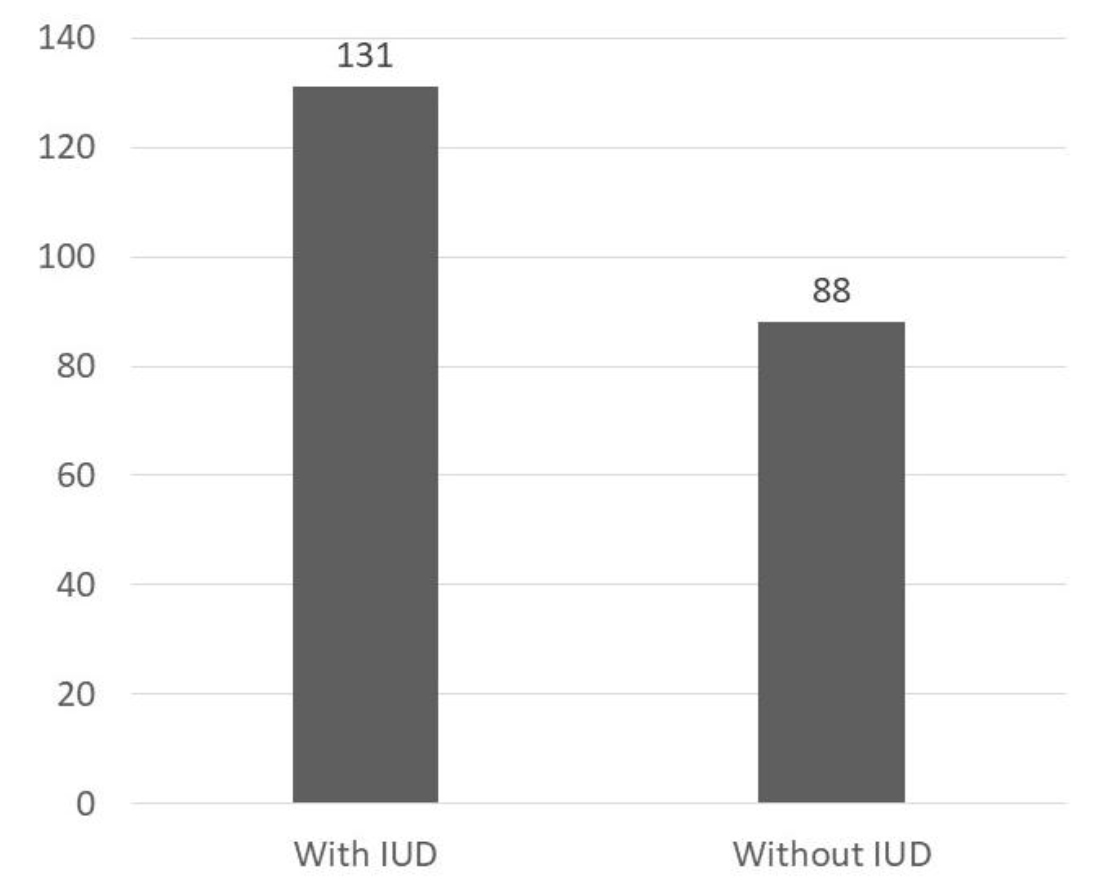
Figure 3. Use of Intrauterine Device (IUD)
The clinical presentation among the patients at the time of the diagnosis was 214 patients (96.83%) presented pain and 202 patients (91.4%) presented vaginal discharge. 139 patients (63%) received a double antibiotic scheme and 57 patients (26%) received a triple antibiotic scheme. Of the patients who received a double treatment scheme, 38 patients (17.19%) were treated with cephalothin and metronidazole, 33 patients (14.9%) with cephalothin and gentamicin, 31 patients (14.03%) with doxycycline and metronidazole, 19 patients (8.6%) with clindamycin and gentamicin, 8 patients (3.62%) with clindamycin and metronidazole, 6 patients (2.71%) with gentamicin and metronidazole, 4 patients (1.81%) with levofloxacin and metronidazole (Figure 4).
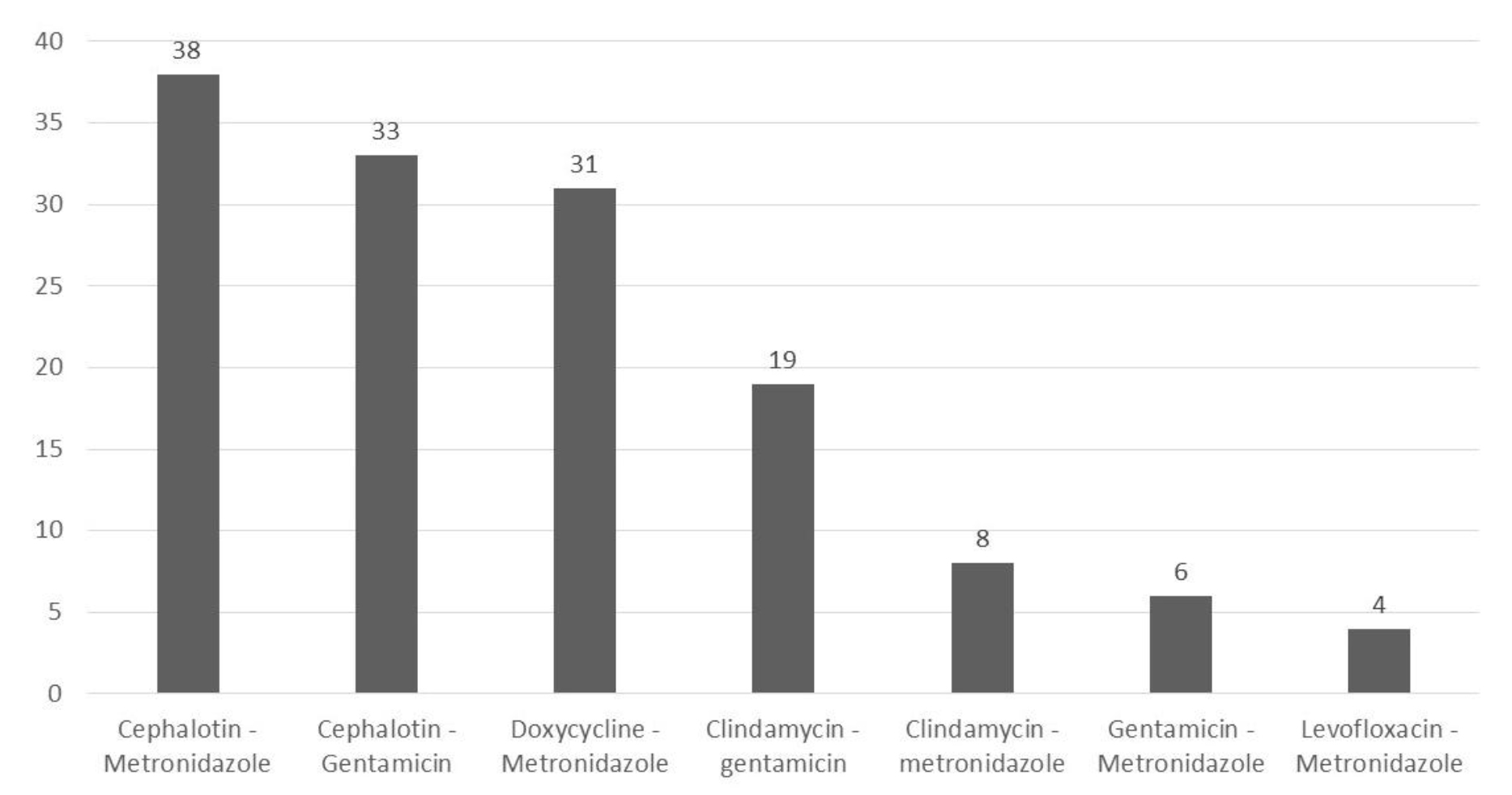
Figure 4. Double antibiotic Scheme
Of the patients who received a triple antibiotic scheme, 28 patients (12.67%) were treated with cephalothin; gentamicin and metronidazole, 8 patients (3.62%) with ceftriaxone, metronidazole and levofloxacin, 7 patients (3.17%) with ampicillin, gentamicin and metronidazole, 5 patients (2.26%) with ceftriaxone, clindamycin and gentamicin, 5 patients (2.26%) with ceftriaxone, gentamicin and metronidazole and 4 patients (1.81%) with cephalothin, doxycycline and metronidazole (Figure 5).
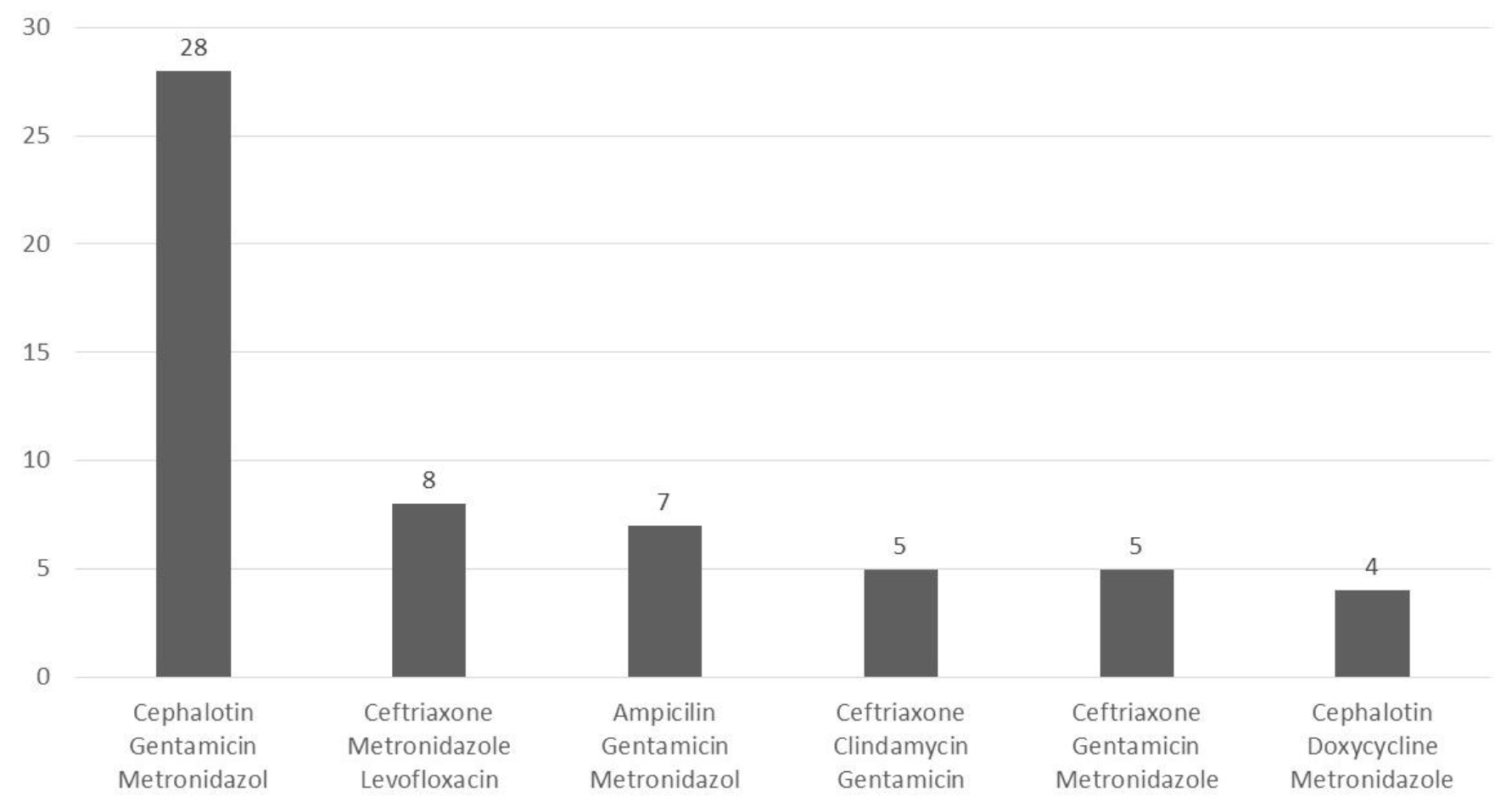
Figure 5. Triple antibiotic Scheme
84 patients underwent a surgical procedure. 20 patients (9.05%) underwent a left salpingoophorectomy, 12 patients (5.43%) had an abdominal hysterectomy plus bilateral salpingoophorectomy, 11 patients (4.98%) had an abdominal hysterectomy, 9 patients (4.07%) had an abdominal washout. In addition, 8 patients (3.62%) underwent an abdominal hysterectomy plus right salpingoophorectomy, 8 patients (3.63%) had a left salpingectomy, 7 patients (3.17%) a right salpingoophorectomy, 6 patients (2.71%) underwent a right salpingectomy and 3 patients (1.36%) underwent abdominal hysterectomy plus left salpingoophorectomy (Figure 6).
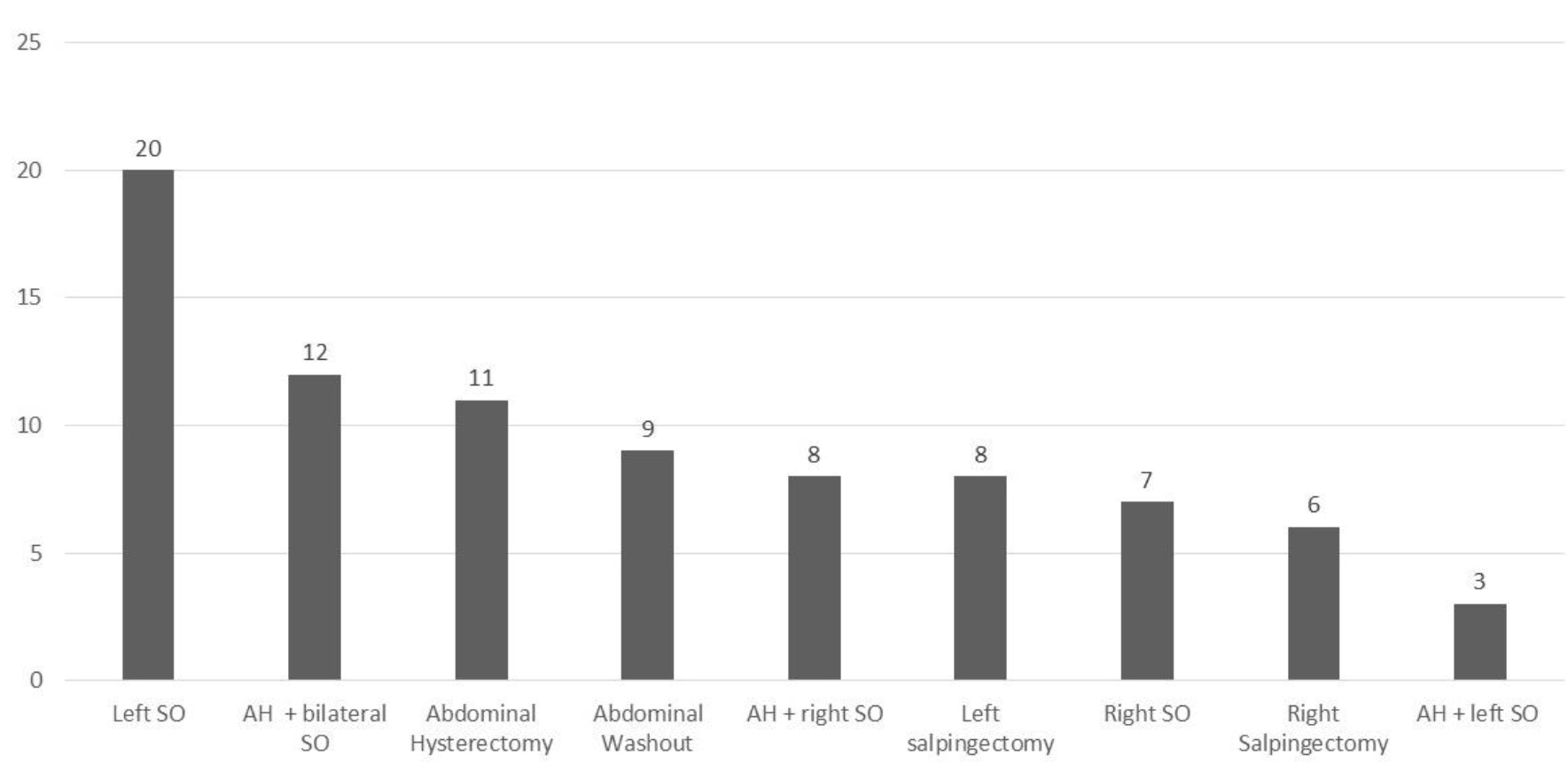
Figure 6. Surgical Procedure. SO, Salpingoophorectomy; AH, Abdominal Hysterectomy.
Discussion
The risk factors for pelvic inflammatory disease are well known and include multiple sexual partners, women under 25, and sexually transmitted diseases [5, 6]. In our study, it was decided to analyze the characteristics of the patients who come to the clinic and they are diagnosed with PID. We found that the average age of patients is 26 to 33 years, age range that differs from other studies, where adolescents or women under 20 years are reported [7]. It has been described that one of the biggest risk factors for PID is the number of sexual partners [8–10]. The results in our study were not very different from what is reported in the literature, because we found that 93 patients had had 2 to 3 sexual partners. Tabacco L. et al. conducted a study on sexual behavior and the relationship between the number of sexual partners and the risk of developing PID. They found that most patients mention only having one sexual partner, causing condom use to decrease and thereby increasing the risk of a sexually transmitted disease [11]. This could explain the case for the 73 patients with only one sexual partner and a diagnosis for PID.
The intrauterine device is one of the most commonly used contraceptives in the population and is one of the risk factors for PID. Data from 12 randomized IUD studies, including more than 20,000 women and more than 5,000 women between 15 and 24 years showed a general PID rate of 1.6 cases per 1,000 women-years of use. After adjustment for confounding variables, the risk of PID rose only during the 20 days immediately after IUD insertion. Although the risk in the first 20 days after insertion was six times the baseline risk, the absolute risk of PID was small and cases of PID were unusual. After the insertion period, the risk of PID for all women returned to the initial risk during the next 8 years of follow-up study. The risk of PID in IUD users was inversely related to age, a finding probably related to a higher prevalence of STIs in younger women rather than the presence of an IUD [12].
In our study, 131 patients mentioned using the IUD as their contraceptive method of choice. However, the question remains if the insertion of the IUD was in a range of 4 months prior to the presentation of the symptoms of PID to be able to relate whether the IUD was the factor risk that in most cases caused the onset of symptoms. The polymicrobial etiology of PID is clearly accepted, so it must be treated with antibiotics that offer coverage against a broad spectrum of pathogens, the CDC has developed guidelines for treatment focused on the most common pathogens, Chlamydia trachomatis and Neisseria gonorrhoeae [13]. We conclude that in our hospital different treatment schemes are used, the most frequent was a double scheme of medications with cephalothin and metronidazole, prescribed scheme in 38 patients that differs from what the literature recommend. The CDC recommends a clindamycin and gentamicin scheme, which in our study was only prescribed in 19 patients, both groups with favorable clinical results. Regarding the triple scheme, the CDC recommends a combination of ceftriaxone, doxycycline and metronidazole or cefoxitin, doxycycline and metronidazole; The triple scheme prescribed more frequently in our study differs from what the CDC recommends because in 28 patients it was decided that cephalothin, gentamicin and metronidazole would be prescribed, a scheme with which favorable results were obtained.
Conclusion
With these results, we were able to know the epidemiological characteristics of the patients diagnosed with pelvic inflammatory disease. Knowing these characteristics, we can carry out programs to detect risk factors and prevent the incidence and recurrence of PID, in addition to find the treatment scheme that has worked best according to the characteristics of our population.
References
- Hernández Durán D, Diaz Mitjans O (2010) Enfermedad inflamatoria pélvica. Revista Cubana de Obstetricia y Ginecología 36: 613–631.
- Risser JM, Risser WL, Risser AL (2008) Epidemiology of infections in women. Infectious disease clinics of North America 22: 581–599.
- Bender N, Herrmann B, Andersen B, Hocking JS, van Bergen J, et al. (2011) Chlamydia infection, pelvic inflammatory disease, ectopic pregnancy and infertility: cross-national study. Sexually transmitted infections 87: 601–608.
- Villacreses S, Stefania S (2013) Prevalencia de las infecciones de transmisión sexual en mujeres de edad fértil, diagnosticadas por medio de estudios citológicos. Estudio realizado en Hospital Enrique C. Sotomayor de septiembre 2012 a febrero del 2013.
- Peláez Mendoza J (2012) Enfermedad inflamatoria pélvica y adolescencia. Revista Cubana de Obstetricia y Ginecología 38: 64–79.
- Barrantes S (2015) Enfermedad Pélvica Inflamatoria. Ginecologia y Obstetricia Revista Médica de Costa Rica y Centro America LXXII 614) 2015: 105–109.
- Valdés S, Essien J, Saavedra D, Bardales J (2006) Enfermedad inflamatoria pelviana en adolescentes. Clínica e Investigación en Ginecología y Obstetricia 33: 177–179.
- Bohm MK, Newman L, Satterwhite CL, Tao G, Weinstock HS (2010) Pelvic inflammatory disease among privately insured women, United States, 2001–2005. Sexually transmitted diseases 37: 131–136.
- Kreisel K (2017) Prevalence of pelvic inflammatory disease in sexually experienced women of reproductive age – United States, 2013–2014. Mobitdity and Mortality Weekly Report 66: 80–83.
- Trent M, Chung SE, Burke M, Walker A, Ellen JM (2010) Results of a randomized controlled trial of a brief behavioral intervention for pelvic inflammatory disease in adolescents. Journal of pediatric and adolescent gynecology 23: 96–101.
- Tabacco (2018) Relationship Status and Sexual Behaviors in Post- Pelvic Inflamatory Disease (PID) Affected Urban Young Women: A Sub-Study of Randomized Controlled Trial. In Arch Nurs Health Care. 4: 088.
- Farley TMM, Rowe PJ, Meirik O, Rosenberg MJ, Chen JH (1992) Intrauterine devices and pelvic inflammatory disease: an international perspective. The Lancet 339: 785–788.
- Workowski KA, Berman SM (2007) Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clinical Infectious Diseases 1: 73–76.