Abstract
Temporomandibular Disorders (TMD) are the most prevalent cause of facial pain without a clear etiopathogenesis and gold standard treatment. There is not an agreement on treatments which involve surgical or conservative interventions. Between the different types of conservative treatments the Fascial Manipulation® could be a promising therapy. Here we describe the case of a patient with orofacial pain that was treated successful with three single sessions of Fascial Manipulation®.
Keywords
TMJ, Fascial Manipulation®, Orofacial pain.
Introduction
Orofacial pain is a heterogeneous group of musculoskeletal and neuromuscular conditions involving the temporomandibular joint complex, surrounding musculature and osseous components [1]. Between these, Temporomandibular Disorders (TMD) are the most prevalent cause of orofacial pain. TMD are highly prevalent and debilitating conditions involving the head and face, with pain affecting the jaw, ears, eyes and frequently causing headache and neck pain [2]. The etiology of chronic TMD is multifactorial and include structural, functional, environmental, social and psychological factors [3]. The prevalence of orofacial pain is between 3% and 12% and is, at least, twice as prevalent in women as men [4]. Musculoskeletal structures disorders include myalgia, usually presents as a dull aching pain due to continued muscle tension, Myofascial Pain (MFP) also presents as a dull, continuous aching pain that varies in intensity. MFP produces pain upon palpation that is local and may refer to other sites, as mapped out by Simons [5]. MFP tends to be seen in muscle pain conditions of a more chronic nature, in which the tension is unremitting. Trigger points can often be seen in MFP and may be localized to a taut band of muscle.
In the literature, treatments for TMD include patient education, home care programs, physical therapy, musculoskeletal manual approach, pharmacotherapy, Non Steroidal Anti-Inflammatory drugs (NSAIDs), local anesthetics, intracapsular injection of corticosteroids, muscle relaxants, antidepressants, occlusal appliance therapy, occlusal adjustment. Surgical care is only indicated when non-surgical therapy has been ineffective [6]. However, the multifactorial pathophysiology of TMJ related pain is far from being completely understood and effective management of pain has not been established yet [7]. Unfortunately, despite the evidence of two systematic reviews that support manual therapy to produce favorable outcomes in TMD [8, 9] the real effectiveness of different types of manual therapy in TMD remains unclear. A manual therapy named Fascial Manipulation® is shown in a preliminary study to be effective in improving tmj disorder when compared to botulin toxin [10]. Here we present to case of a patient with chronic tmd disorder treated successfully treated with Fascial Manipulation.
Case report
A 65 years old woman, mixed race, Brazilian was assessed and treated at the TMD clinic of the Faculty of Dentistry, State University of Rio de Janeiro (UERJ). She complained of orofacial pain and difficulties chewing and eating for the last 25 months, with concomitant neck pain and an history of headache lasting more than 5 years. She referred a history of whiplash following a car accident that occurred 7 years ago.
The patient has undergone many months of physical therapy without significative improvement and she has been using an Oral Appliances (OAs) (also known as flat plane stabilization appliance, Michigan splint, muscle relaxation appliance or gnathologic splint) for the last 6 months. Pain was described as constant, burning sensation severe enough to affect sleeping. Perceived pain was assessed with the Visual Analogue Scale (Vas) and scored as 9 on a 0–10 scale (Table 1) The RDC/TMD was utilized as the gold-standard instrument and performed by a sole examiner, trained and calibrated according to specifications established by the International RDC/TMD Consortium. At the initial examination it was recorded the occurrence of TMJ clicking, crepitus, or jaw opening interferences with or without pain. The clinician viewed the patient’s opening and closing patterns to note any mandibular deviations. The evaluation of mandibular ROM consisted of measuring comfort opening, unassisted opening, assisted opening, with a millimeter ruler while noting the severity and location of pain with jaw movement (Table 2) The EMG evaluation of the temporalis and masseter muscles during maximum voluntary contraction (tooth clenching) were carried out using the New miotool (MiotecEquipamentosbiomédicosltda, Petrópolis, Porto Alegre, RS, Brasil) with 14-bit resolution and a sampling frequency of 2000 Hz, IRMC > 126 dB and signal noise rate < 2 LSB, Security insulation 3000 V(rms) (table 3). All procedures were performed three times, with a thirty seconds interval between isometric contractions to avoid muscle fatigue. After electromyography signal acquisition, all the data were processed in Miotec Suite (MiotecEquipamentosbiomédicosltda, Petrópolis, Porto Alegre, RS, Brasil) to analyse the root square mean (RMS) in µV. All the evalution were carried out before the Treatment (T0), after the treatment (T1) and at 3 months follow up (T2). On physical examination the range of motion of the neck (ROM) was limited in the sagittal plane (neck flexion) and on the frontal plane (lateral flexion). The palpatory verification of the CC and CF was carried out according to the Stecco’s method (reference) on the following segments: thorax (TH), Scapula (SC), Neck (CL), Head (CP2, CP3) to identify the densified points (Figure 1). The points are selected after a specific assessment process, guided by a specific chart (FM chart) [11] involving medical record, clinical examination of specific movements and palpatory verifications. Palpation evaluates patient pain rate, radiation and most important, the presence of tissue stiffness, call “densification” [12]. During the clinical history, the segments in dysfunction are identified with an emphasis on the chronology to permit the development of an hypothesis based on the current symptomatology of patients and previous musculoskeletal events, which may be causing compensations. In Fascial manipulation the therapist use the elbow and knuckles generating a deep friction for 3–5 minutes over each point.
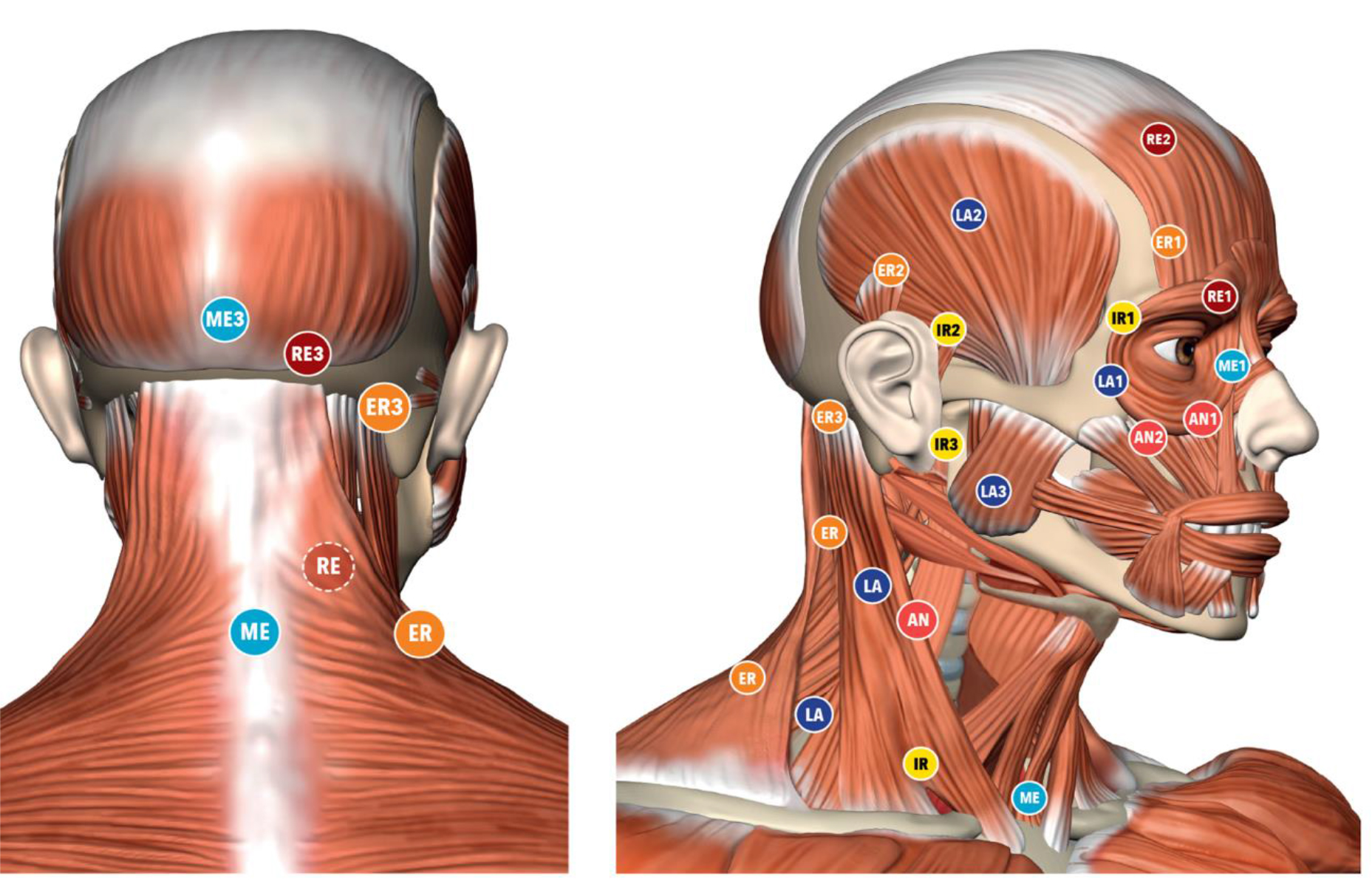
Figure 1. Location of the Center of Coordination points
The treatment are applied over specific points, call Center of Coordination (CCs) and Center of Fusion (CFs), that are anatomically safe because do not overlie major superficial nerves and veins. Additional guidance for point selection includes avoiding the patients’ excessively painful areas where inflammation, lesions or even fractures could be present. The patient underwent three weekly session of Fascial Manipulation® of 1 hour. The VAS scale, between initial condition (T0) and after the treatment (T1) was maintained at 3 month follow up (T2) (Table 1). The patients passed from the symptomatic condition (VAS 9) to asymptomatic (VAS 1) after the treatment. The comfortable without pain opening of the mounts improved (Table 2). Un-assistant and assistant opening improved after treatment, at T1 and T2 follow up. In the table 3 are presented the value of the isometric contraction which improved for the masseter and temporalis muscles bilaterally.
Table 1. VAS T0 = VAS before treatment; T1 = VAS after treatment; T2 = VRS after 3 months
|
|
VAS |
|
T0 |
136.56 |
|
T1 |
264.60 |
Discussion
In the light of our case report, Fascial Manipulation® can improve pain, function and myoelectrical activity in patient with orofacial pain. FM was able to diminish the articular loading on the TMJ which translate in a better mandibular kinematics with less muscle pain. Even if FM share some similarity with other techniques, it presents a different rationality and clinical approach. While the deep friction can be compared to other techniques, the reasoning behind the choice of points treated presents major differences. The points are selected after a specific assessment process involving clinical history taking, a clinical examination of specific movements as well as palpatory verifications [12, 11]. Apart from the use of clinical procedures (palpation, auscultation, measuring of active and passive mandibular mobility), FM requires additional orthopedic tests that implies a modern, biomedical approach, thanks to the knowledge of the human fascial system, but, at the same time, uses an individual approach to the patient as recommended by many Authors [13–15].
Table 2. Assisted: maximum opening with help, unassisted: maximum opening without help. T0 = before treatment; T1 = after treatment; T2 = 3 months;
|
|
Comfortable |
Unassisted opening |
Assisted opening |
|
T0 |
32,51 |
45,30 |
49,23 |
|
T1 |
42,33 |
51,14 |
54,08 |
|
T2 |
40.1 |
48,18 |
50,75 |
Table 3. EMG evaluations of the masticatory muscles in isometric contraction T0= before treatment; T1= after treatment; T2= 3 months
|
|
Right |
Left Masseter |
Right Temporal |
Left |
|
T0 |
136.56 |
176.27 |
154.45 |
127.50 |
|
T1 |
264.60 |
260.75 |
221.47 |
159.61 |
|
T2 |
411.61 |
427.30 |
279.65 |
215.82 |
Conclusion
FM could be used as an effective method for facial pain being a rapid, safe and cost effective approach to reduce pain and gain function and mouth opening that can be used before occlusion stabilization appliance. We suggest further studies that compare the combined treatment of FM with temporomandibular disorder treatment in patient with TMD in a Randomized Controlled Trial (RCT).
References
- McNeill C (1993) Temporomandibular Disorders: Guidelines for Classification, Assesment, and Management (2nded.). Chicago, IL: QuintessencePublishingCo, Inc.
- Germain L, Malcmacher L (2017) Frontline Temporomandibular Joint/Orofacial Pain Therapy for Every Dental Practice. Compend Contin Educ Dent 38: 299–305. [crossref]
- Fillingim RB, Ohrbach R, Greenspan JD, Knott C, Diatchenko L et al. (2013) Psychological factors associated with development of TMD: the OPPERA prospective cohort study. J Pain 14: T75–T90. [crosssref]
- Okeson JP (2005) Bell’s Orofacial Pains. The Clinical Management of Orofacial Pain (6th ed.). Carol Stream, IL: Quintessence Publishing Co, Inc.
- Simons DG, Travell JG (1999) Myofascial Pain and Dysfunction: The Trigger Point Manual. Vol 1. Baltimore: Williams & Wilkins.
- Romero-Reyes M, Uyanik JM (2014) Orofacial pain management: current perspectives. J Pain Res 7: 99–115. [crossref]
- Lin CS (2014) Brain signature of chronic orofacial pain: a systematic review and metaanalysis on neuroimaging research of trigeminal neuropathic pain and temporomandibular joint disorders. PloS One 9: e94300. [crossref]
- McNeely ML, Armijo Olivo S, Magee DJ (2006) A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther 86: 710–725. [crossref]
- Medlicott MS, Harris SR (2006) A systematic review of the effectiveness of exercise, manual therapy, electrotherapy, relaxation training, and biofeedback in the management of temporomandibular disorder. Phys Ther 86: 955–973. [crossref]
- Guarda-Nardini L, stecco A, Stecco C, Masiero S, Manfredini D (2012) Myofascial Pain of Jaw Muscles: Comparison of Short-Term Effectiveness of Botulinum Toxin Injections and Fascial manipulation technique. The Journal of Craniomandibular Practice 30: 95–102. [crossref]
- Pintucci M, Simis M, Imamura M, Pratelli E, Stecco A et al. (2017) Successful treatment of rotator cuff tear using Fascial Manipulation® in a stroke patient. Journal of Bodywork & Movement Therapies 21 653–657. [crossref]
- Day JA, Copetti L, Rucli G (2012) From clinical experience to a model for the human fascial system. J Bodyw Mov Ther 16: 372–80.
- Kordaß B, Fasold A (2012) ManuelleStrukturanalyse. Teil 1: Grundlagen und klinischeUntersuchung. ZWR 212: 8–11.
- Badel T, Krapac L, Kraljević A (2012) The role of physical therapy in patients with temporomandibular joint disorder. FizRehabil Med 24: 21–33.
- Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M et al. (2011) Temporomandibular disorders and associated clinical comorbidities. Clin J Pain 27: 268–274.
- Schulze W. Therapeutic communication with CMD patients – Part 2. J Craniomandib Funct 2010; 2: 149–60.