Abstract
One way of reducing the cost for screw-retained implant-supported dental prosthesis is to avoid the use of prosthetic abutments. However, concerns have been raised that this might lead to complications such as extensive marginal bone loss resorption and implant loss. The aim of the study was to retrospectively evaluate a cohort of consecutive patients treated with implant-level prosthetic constructions after 5 years in function. A total of 49 consecutive patients previously treated with 102 hydrophilic dental implants (Neoss Proactive, Neoss Ltd, Harrogate, UK) in two private dental clinics were included in the study. Fifty-four implants were installed in maxillae and 48 in mandibles to replace single teeth (n = 21), to support partial bridges (n = 26), total maxillary bridges (n = 2), or mandibular overdentures (n = 2). The majority of patients (n = 37) had implants placed in healed sites without any adjunctive procedures. In 12 patients, implants were immediately placed in extraction sockets or in conjunction with maxillary sinus floor augmentation. A submerged healing period of 3 to 4 months was used before healing abutments were connected to the implants. Impressions were taken after 7 to 10 days. Baseline (abutment connection surgery), 1- and 5-year intraoral radiographs were used to measure marginal bone levels and calculate bone loss. Two mandibular implants were lost (2%) during the 5 years in function. The average marginal bone loss amounted to 0.7 ± 0.7 mm after 1 year and 0.9 ± 1.1 mm after 5 years. There was no correlation between insertion depth and bone loss. It is concluded that the use of screw-retained implant-level prosthetic constructions resulted in high implant survival rate and minimal marginal bone loss after 5 years in function.
Keywords
Dental Implants, Follow-Up Study, Implant-Level, Marginal Bone Resorption, Screw-Retained Prosthesis
Introduction
Dental implants is a first choice treatment modality for replacement of missing teeth and an integrated part of treatment planning and also executed in many modern dental clinics. The patients expect a rapid and affordable treatment with a long-lasting result with few complications during clinical function. One way of reducing costs for the patient is to avoid the use of costly prosthetic abutments and hence attaching the screw-retained prosthetic construction directly to the implant [1]. However, authors have argued that more complications may be seen without the use of prosthetic abutments. For instance, experimental studies have demonstrated that the presence of a micro-gap near the marginal bone may result in bone resorption due to violation of the “biological width” [2]. Moreover, repeated detachment of healing abutments, i.e. repeated insults to the “biological width”, resulted in marginal bone resorption in another animal study [3]. Some authors have suggested that implant-level prosthetic constructions are predisposed to inaccuracy and misfit, which could result in unfavourable stresses and strains leading to screw fracture, framework fracture, implant fracture, marginal bone loss, and even implant loss [4]. Indeed, clinical studies have shown less marginal bone resorption at implants with than without prosthetic abutments [4, 5]. For instance, Toia et al demonstrated significantly less marginal bone loss at implants with (0.005 mm) than without (0.086 mm) abutments after one year of function. However, as the difference was less than one tenth of a millimetre. It can be argued that the difference in that study was not clinically relevant. Other studies have shown good clinical outcomes and few complications with implant-level restored implants [6].
The Neoss implant system was introduced without the use of prosthetic abutments. The implant has a 1.9 mm high collar, which can be fully submerged or left above the bone level. Impressions are taken at implant level and healing abutments used between appointments. The final construction is screw-retained directly to the implant(s) through a flat-to-flat connection using a torque of 30 Ncm with no other attempts to seal the micro-gap. Thus, depending on the level of submerging the prosthesis/implant gap is theoretically violating the biological width, which according to the theories described above may result in marginal bone loss. Previous studies on this implant design with a smooth surface topography (Bimodal) have shown minimal bone resorption after 1 to 5 years of follow-up [7, 8]. Since 2009 the Neoss implant has a hydrophilic surface produced by blasting and acid-etching. Short-term studies have demonstrated small changes of the marginal bone levels during the first year in function [9, 10]. However, no long-term studies have yet been performed.
The aim of the investigation was to study the 5-year implant survival and changes of marginal bone levels in a group of consecutive patients treated with hydrophilic implants and implant level screw-retained fixed constructions.
Materials and Methods
A total of 49 consecutive patients previously treated with 102 hydrophilic dental implants (Neoss Proactive, Neoss Ltd, Harrogate, UK) in two private dental clinics were retrospectively evaluated with regard to survival rate and marginal bone loss after five years of loading (Table 1). The surgical and prosthetic procedures and one-year outcomes of the same patient group have been presented in detail in a previous publication [9]. All patients had been thoroughly informed and gave their written consent to the proposed therapy and follow-up routines including annual check-ups. No extra measures were taken for the purpose of the study. For quality assurance purposes, all implant treatments in the clinics are routinely documented using a computerized system (MS Excel, MicroSoft, Redmond, USA) from which the data used in the study could be extracted. The study followed the directives given by the Ethical Committee at the Feltre Hospital, Feltre, Italy and in accordance with the World Medical Association Declaration of Helsinki.
Table 1. Type and number of implants used in the study. Failed implants within parentheses.
|
Implant diameter |
Implant length |
Total |
||||
|
7 mm |
9 mm |
11 mm |
13 mm |
15 mm |
||
|
3.5 mm |
|
1 |
1(1) |
1 |
|
3 |
|
4.0 mm |
|
14 |
29 |
23 |
7 |
73 |
|
4.5 mm |
1 |
4 |
6 |
2 |
|
13 |
|
5.0 mm |
|
7(1) |
6 |
|
|
13 |
|
Total |
1 |
21 |
42 |
25 |
7 |
102 |
Fifty-four of the 102 implants were installed in maxillae and 48 in mandibles to replace single teeth (n = 21), to support partial bridges (n = 26), total maxillary bridges (n = 2), or mandibular overdentures (n = 2) (Table 2).
Table 2. Type of prosthetic constructions.
|
|
Mandible |
Maxilla |
|
Single tooth replacement |
12 |
9 |
|
Fixed partial prosthesis |
12 |
14 |
|
Fixed total prosthesis |
2 |
– |
|
Overdenture |
– |
2 |
The majority of patients (n = 37) had implants placed in healed sites without any adjunctive procedures. In 12 patients, implants were immediately placed in extraction sockets or in conjunction with maxillary sinus floor augmentation. A submerged healing period of 3 to 4 months was used before healing abutments were connected to the implants. Impressions were taken after 7 to 10 days. All prosthetic constructions were screw-retained on implant level without the use of abutments (Figure 1).
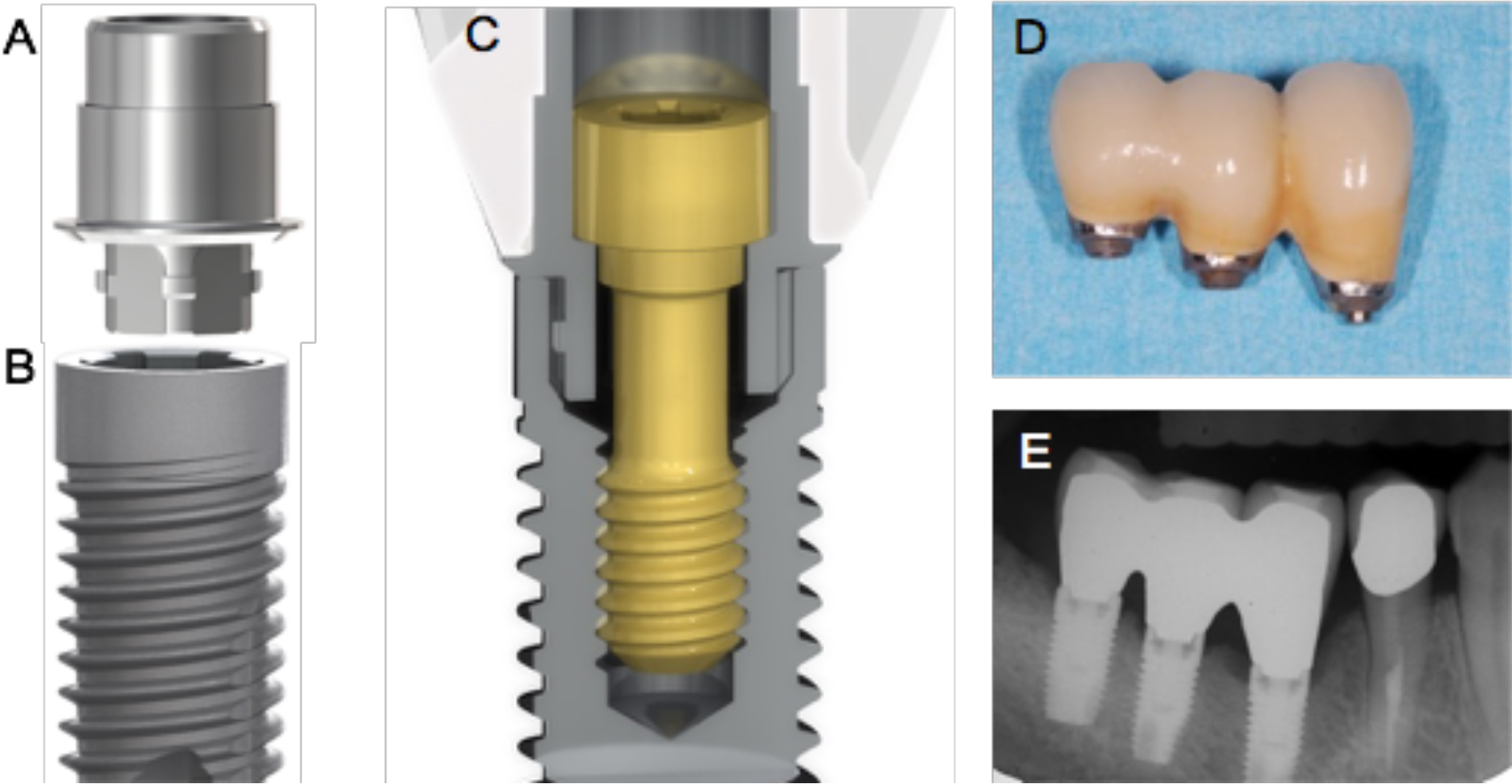
Figure 1. Showing the prosthetic connection of the Neoss implant system. A. The NeoLink component. B. Implant C. Crossection through a single crown, NeoLink with prosthetic goldscrew and implant. D. Clinical and E. radiographic view of an implant-level three-unit bridge.
Baseline (abutment connection surgery), 1- and 5-year intraoral radiographs were used to measure marginal bone levels and calculate bone loss. Only implants with measurements from all three time points were used for calculations. The upper corner of the coronal shoulder of the implant was used as reference point, and measurements from the reference point to the first bone contact at the mesial and distal aspects of the implant were performed using a PC and specially designed software (Image-J, National Institutes of Health, Bethesda, MD, USA) (Figure 2). A mean value was calculated for each implant and time point.

Figure 2. Radiographs of the same case at baseline and after 1 and 5 years of follow-up. The mesial implant shows some bone loss, while the distal implant show no bone loss.
The Spearman correlation test was used to evaluate a possible correlation between depth of implant placement and marginal bone loss after 5 years. A significance level p<0.05 was used for the test.
Results
Two implants were lost, giving a cumulative survival rate (CSR) of 98.0% after 5 years. Both failures occurred in the posterior mandible and all maxillary implants were successful (Table 1). One implant (3.5/11 mm), which had been accidentally placed close to a neighbouring root, was removed after 3 months of loading. The patient could maintain the partial bridge on two implants and a new implant was inserted after healing and eventually connected to a new bridge. The second failed implant (5/9 mm) was removed during the fifth year due to marginal bone loss, suppuration and discomfort.
The radiographs from a total of 79 implants (77.5% of all implants) could be measured at baseline, after one and five years (Figure 3). The marginal bone levels were situated 0.3 ± 0.4 mm, 1.0 ± 0.6 mm and 1.2 ± 1.0 mm below the implant shoulder at baseline and after 1 and 5 years, respectively (Table 3). The average marginal bone loss amounted to 0.7 ± 0.7 mm with 3.8% of the implants showing more than 2 mm and no implant more than 3 mm bone loss after 1 year (Table 3). After 5 years, the average bone loss was 0.9 ± 1.1 mm with 3.8 % of implants showing more than 2 mm bone loss and 3.8% more than 3 mm bone loss (Table 3). The majority of implants showed bone level gain (34.2%) or no and up to 1 mm of bone loss (55.7) from the 1st to the 5th year (Table 3). There was no correlation between insertion depth and bone loss.
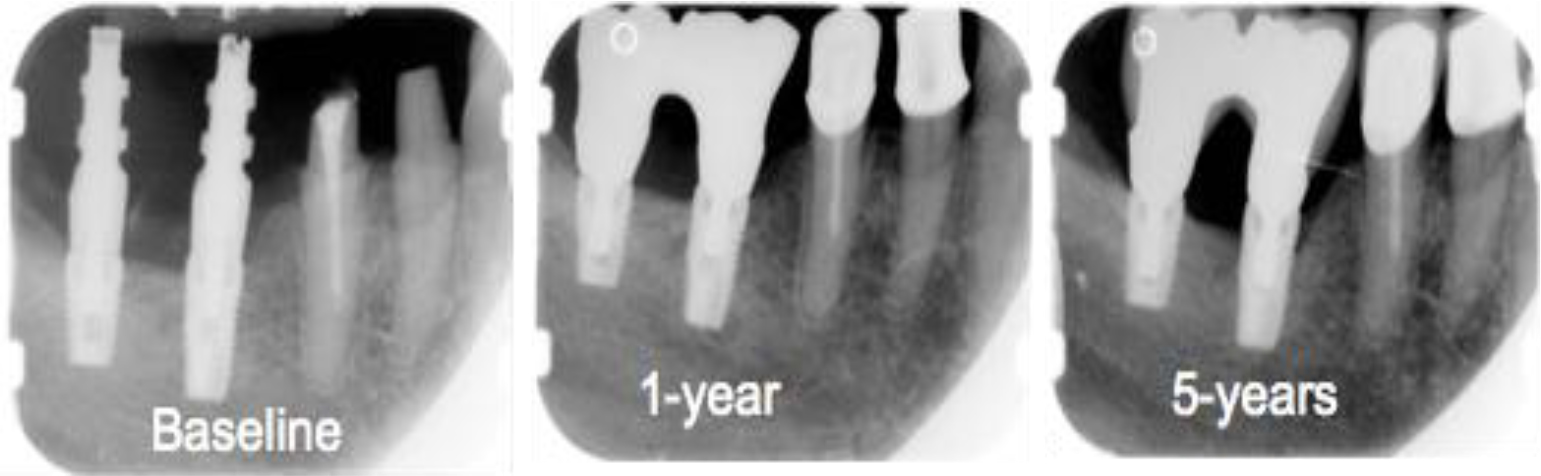
Figure 3. Schematic showing the reference point for bone level measurements. The collar of the implant is 1.9 mm.
Table 3. Marginal bone level and bone resorption based on 79 implants with readable radiographs from all three time points.
|
|
Baseline |
1 year |
5 years |
|
Bone level |
0.3 ± 0.4 |
1.0 ± 0.6 |
1.2 ± 1.0 |
|
Bone loss |
|
0.7 ± 0.7 |
0.9 ± 1.1 |
|
Frequency of bone loss |
n (%) |
n (%) |
|
|
< 0 mm |
8 (10.1) |
11(13.9) |
|
|
0–1 mm |
49 (62.0) |
41 (51.9) |
|
|
1.1–2 mm |
19 (24.1) |
21 (26.6) |
|
|
2.1–3 mm |
3 (3.8) |
3 (3.8) |
|
|
> 3 mm |
0 |
3 (3.8) |
|
Discussion
The present study group was evaluated after one year and the results presented in a previous publication, where one implant failure was reported9. The present follow-up showed one additional implant failure giving a total implant survival rate of 98.0 % after five years of function. This is in line with the outcomes from 5-year follow-up studies of the same and other modern dental implant systems [8, 11–13].
Only one of the failures was related to the performance of the implant as the first failure was due to a surgical mistake. The second implant was removed due to extensive marginal bone loss, suppuration and discomfort. The infection occurred during the 5th year of function after a continuous slow and asymptomatic bone loss from implant placement. This implies that the reason for bone loss was other than infection, which likely was a secondary phenomenon. This is in accordance with another publication in where causes for marginal bone resorption were discussed [14]. Other authors have argued that bone loss at implants is biofilm-mediated and advocate the use of periodontal indices to diagnose mucositis and peri-implantitis in analogy with gingivitis and periodontitis at teeth [15]. However, a recent review could not find any evidences that probing is an effective means of diagnosing peri-implant disease or predicting implant failure [16]. In contrast, the authors expressed concerns that the use of probing could lead to over-diagnosis of disease and unnecessary treatment of healthy implants. Nevertheless, also when applying liberal definitions of peri-implant infection [17] the condition requiring removal of the implant in the study can be judged as “peri-implantitis”. Hence, peri-implantitis was seen in 1% of the implants of the present study. Based on a previous literature search, the frequency of implants with reported peri-implant infection and significant bone loss leading to implant removal or other surgical intervention was on average 2.7% after 7 to 16 years [18].
Only implants with radiographs available from all observation time points were evaluated with regard to marginal bone levels in the present study. The present authors believe this results in more accurate data than using mean values from all available radiographs from the different time points. Some marginal bone remodelling was observed during the first year of function followed by a minor further change up to the fifth year check-up, which is in line with many other studies [12, 19]. The average marginal bone loss amounted to 0.7 ± 0.7 mm after 1 year and 0.9 ± 1.1 mm after 5 years. The majority of implants showed bone level gain (34.2%) or no and up to 1 mm of bone loss (55.7) from the 1st to the 5th year.
Our study showed less bone loss than in a previous study, where Brånemark implants with and without prosthetic abutments were evaluated after 5 years [20]. In their comparative investigation, the least amount of bone loss was found at implants with a machined-surfaced abutment after 5 years. The bone loss amounted to 1.6 mm compared to 0.9 mm in our study in spite of using implant-level prosthetic constructions. However, it should be pointed out that our baseline radiographs where taken at abutment or prosthesis connection and that implant surgery was used as baseline in the Göthberg et al study [20]. Therefore, any bone loss occurring from surgery to our baseline was not accounted for. However, the mean marginal bone level was still located more coronal in our study after 5 years, i.e. 1.2 mm vs 1.6 mm. An average of 0.2 mm of marginal bone was lost from the 1st to the 5th year in the present study, while about 0.6 mm was lost when pooling all implants in the Göthberg et al study [20]. Interestingly, the least bone loss from the one to the five-year follow-up was seen for implants restored at implant level in that study, indicating that most of the changes occurred during the first year in function [20]. In a comparative study using AstraTech implants, the bone loss at implants with or without prosthetic abutments was less than 0.1 mm after one year [4]. However, since there was a statistically significant difference in favour of the use of abutments together with less bleeding on probing, the authors argued that it is safer to use abutments rather than restoring the implants at implant level. However, in light of the discussion above neither initial bone loss nor the presence of bleeding on probing seems to reflect or predict clinically relevant problems and, according to the present authors, the use of prosthetic abutments cannot be justified. Moreover, a 5-year clinical follow-up study reported few complications of implant-level restorations [6], which corroborates with our findings.
Continuous marginal bone loss and related long-term complications is an obvious threat to the longevity of an implant and is the main reason why many historical implant designs are not used any longer [21, 22]. It is well known that also different modern implant designs show different amounts of marginal bone remodelling during the first year in function but that small differences are observed from the 1st year and onwards [19]. In a meta-analysis where Straumann, Brånemark and AstraTech implants were analysed based on published 5-year follow-up studies, all three designs seemed to result in excellent long-term outcomes in spite of measureable differences of initial marginal bone loss [12]. Hence, steady marginal bone levels after the first year seems more important than the amount of bone that is lost during the first year. So if the goal is to minimize initial marginal bone resorption, the choice of implant seems more effective than if using prosthetic abutments or not. This is also exemplified by the studies by Toia et al [4] and Göthberg et al [20], which showed greater differences between implant systems than between prosthetic protocols.
Implant placement depth did not have any effect on marginal bone resorption in the present study. This is in contrast to a 5-year study on Nobel Replace implants, where less bone loss was reported if the 2 mm smooth surfaced collar was placed above below the bone level compared to implants placed at or below the bone level [23]. The bone level shifted to the first thread for all implants over time, which indicated that the smooth surfaced collar could not retain the bone. It is likely that the surface topography played a role for the maintenance of the bone level at the collar in the present study. However, studies on other implant designs with moderately rough surfaces on the collar have shown both minimal [12] and extensive bone loss [24, 25], which indicates that other factors such as collar geometry and drilling protocols are of equal importance. Since it is difficult to draw general conclusions from one implant type, each individual design needs to be evaluated in clinical follow-up studies. Within the limitations of the present study, it is concluded that the evaluated implant system performs well when restored at implant level.
References
- Hellden LB, Derand T (1998) Description and evaluation of a simplified method to achieve passive fit between cast titanium frameworks and implants. Int J Oral Maxillofac Implants 13: 190–196. [crossref]
- Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D (1997) Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Periodontol 68: 186–198. [crossref]
- Abrahamsson I, Berglundh T, Sekino S, Lindhe J (2003) Tissue reactions to abutment shift: an experimental study in dogs. Clin Implant Dent Relat Res 5: 82–88. [crossref]
- Toia M, Stocchero M, Becktor JP, Chrcanovic B, Wennerberg A (2019) Implant vs abutment level connection in implant supported screw-retained fixed partial dentures with cobalt-chrome framework: 1-year interim results of a randomized clinical study. Clin Implant Dent Relat Res 21: 238–246. [crossref]
- Göthberg C, Gröndahl K, Omar O Thomsen P, Slotte C (2018) Bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-Years RCT with different abutment types and loading protocols. Clin Implant Dent Relat Res 20: 313–321. [crossref]
- Hellden L, Ericson G, Elliot A, Fornell J, Holmgren K, et al. (2003) A prospective 5-year multicenter study of the Cresco implantol-ogy concept. Int J Prosthodont 16: 554–562. [crossref]
- Sennerby L, Andersson P, Verrocchi D, Viinamäki R (2012) One-year outcomes of Neoss bimodal implants. A prospective clinical, radiographic, and RFA study. Clin Implant Dent Relat Res 14: 313–320. [crossref]
- Zumstein T, Billström C, Sennerby L (2012) A 4- to 5-year retrospective clinical and radiographic study of Neoss implants placed with or without GBR procedures. Clin Implant Dent Relat Res 14: 480–490. [crossref]
- Degasperi W, Andersson P, Verrocchi D, Sennerby L (2014) One-year clinical and radiographic results with a novel hydrophilic titanium dental implant. Clin Implant Dent Relat Res 16: 511–519. [crossref]
- Zumstein T, Sennerby L (2016) A 1-Year Clinical and Radiographic Study on Hydrophilic Dental Implants Placed with and without Bone Augmentation Procedures. Clin Implant Dent Relat Res 18: 498–506. [crossref]
- Andersson P, Pagliani L, Verrocchi D, Volpe S, Sahlin H et al (2019) Factors Influencing Resonance Frequency Analysis (RFA) Measurements and 5-Year Survival of Neoss Dental Implants. International Journal of Dentistry 2019: Article ID 3209872, 9 pages.
- Laurell L, Lundgren D (2011) Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res 13: 19–28. [[crossref]
- Derks J, Håkansson J, Wennström JL, Tomasi C, Larsson M, et al. (2015) Effectiveness of implant therapy analyzed in a Swedish population: early and late implant loss. J Dent Res 94: 44–51. crossref]
- Albrektsson T, Dahlin C, Jemt T, Sennerby L, Turri A, et al. (2014) Is marginal bone loss around oral implants the result of a provoked foreign body reaction? Clin Implant Dent Relat Res 16: 155–165. [crossref]
- Lindhe J, Meyle J, Group D of European workshop on periodontology (2008) Peri-implant diseases: Consensus Report of the Sixth European Workshop on Periodontology. J Clin Periodontol 35: 282–285. [crossref]
- Coli P, Christiaens V, Sennerby L, Bruyn H (2017) Reliability of periodontal diagnostic tools for monitoring peri-implant health and disease. Periodontol 2000 73: 203–217. [crossref]
- Albrektsson T, Buser D, Chen ST, Cochran D, DeBruyn H, et al (2012) Statements from the Estepona consensus meeting on peri-implantitis, February 2–4, 2012. Clin Implant Dent Relat Res 14: 781–782.
- Albrektsson T, Buser D, Sennerby L (2012) Crestal bone loss and oral implants. Clin Implant Dent Relat Res 14: 783–791. [crossref]
- Oh TJ, Yoon J, Misch CE, Wang HL (2002) The causes of early implant bone loss: myth or science? J Periodontol 73: 322–333. [crossref]
- Göthberg C, Gröndahl K, Omar O Thomsen P, Slotte C (2018) Bone and soft tissue outcomes, risk factors, and complications of implant-supported prostheses: 5-Years RCT with different abutment types and loading protocols. Clin Implant Dent Relat Res 20: 313–321. [crossref]
- d’Hoedt B, Schulte W (1989) A comparative study of results with various endosseous implant systems. Int J Oral Maxillofac Implants 4: 95–105. [crossref]
- Albrektsson T, Sennerby L (1991) State of the art in oral implants. J Clin Periodontol 18: 474–481. [crossref]
- Pettersson P, Sennerby L (2015) A 5-year retrospective study on Replace Select Tapered dental implants. Clin Implant Dent Relat Res 17: 286–295. [crossref]
- Ostman PO, Hellman M, Albrektsson T, Sennerby L (2007) Direct loading of Nobel Direct and Nobel Perfect one-piece implants: a 1-year prospective clinical and radiographic study. Clin Oral Implants Res 18: 409–418. [crossref]
- Nowzari H, Chee W, Yi K, Pak M, Chung W, et al. (2006) Scalloped dental implants: a retrospective analysis of radiographic and clinical outcomes of 17 Nobel Perfect implants in 6 patients. Clin Implant Dent Relat Res 8: 1–10. [crossref]